Tight calves can be a frustrating and limiting issue. At why.edu.vn, we help you understand why you might be experiencing calf tightness and offer practical solutions to alleviate discomfort and improve lower leg health. Learn about calf tightness now.
1. What Causes Tight Calves?
Calf tightness is a common condition that can affect people of all ages and activity levels. Several factors can contribute to this discomfort, ranging from lifestyle choices to underlying medical conditions. Understanding these causes is the first step in finding effective relief.
1.1. Muscle Overuse
Overuse is a primary cause of tight calves, especially among athletes and individuals who engage in frequent physical activity. When the calf muscles are subjected to repetitive or intense strain without adequate rest and recovery, they can become overworked and develop tightness. This is especially true when suddenly increasing the intensity or duration of physical activity.
- High-Impact Activities: Sports like running, basketball, and tennis involve repetitive calf muscle contractions.
- Prolonged Standing: Jobs that require standing for extended periods can lead to muscle fatigue and tightness.
- Inadequate Warm-Up: Failing to properly warm up the calf muscles before exercise can increase the risk of tightness and injury.
1.2. Muscle Underuse
Conversely, a sedentary lifestyle can also cause tight calves. When the calf muscles are not used regularly, they can become stiff and less flexible. This lack of use can result in decreased blood flow and reduced range of motion, leading to tightness and discomfort.
- Sedentary Jobs: Desk jobs or professions that involve prolonged sitting can contribute to calf tightness.
- Immobility: Periods of inactivity due to illness or injury can result in muscle stiffness and reduced flexibility.
- Lack of Stretching: Failing to incorporate regular stretching into your routine can exacerbate muscle tightness.
1.3. Dehydration
Dehydration plays a significant role in muscle function and flexibility. Water is essential for maintaining muscle elasticity and facilitating proper muscle contractions. When the body is dehydrated, the muscles can become stiff and more prone to cramping and tightness.
- Reduced Blood Volume: Dehydration decreases blood volume, reducing nutrient delivery to muscles.
- Electrolyte Imbalance: Dehydration can lead to electrolyte imbalances, which are crucial for muscle function.
- Increased Muscle Stiffness: Lack of water can cause muscle fibers to become rigid and less pliable.
1.4. Footwear Choices
The type of footwear worn can significantly impact the health and flexibility of the calf muscles. Shoes that restrict natural foot movement or alter biomechanics can contribute to calf tightness.
- High Heels: Wearing high heels shifts the body’s center of gravity, causing the calf muscles to contract and shorten.
- Flat Shoes: Shoes with inadequate arch support can lead to overpronation, affecting calf muscle alignment and function.
- Tight or Restrictive Shoes: Footwear that limits foot movement can reduce blood flow and contribute to muscle stiffness.
1.5. Age-Related Changes
As people age, the natural elasticity of muscles and tendons decreases, leading to reduced flexibility and increased stiffness. Age-related changes in muscle composition and hydration levels can also contribute to calf tightness.
- Decreased Muscle Mass: Muscle mass naturally declines with age, reducing strength and flexibility.
- Reduced Collagen Production: Collagen, a protein that supports muscle and tendon elasticity, decreases with age.
- Lower Hydration Levels: Older adults may experience reduced thirst sensation, leading to chronic dehydration and muscle stiffness.
1.6. Medical Conditions
Certain medical conditions can contribute to calf tightness. These conditions may affect nerve function, blood flow, or muscle health, leading to discomfort and stiffness in the calf muscles.
- Peripheral Artery Disease (PAD): PAD reduces blood flow to the legs, causing muscle pain and tightness.
- Diabetes: High blood sugar levels can damage nerves and blood vessels, affecting muscle function.
- Sciatica: Nerve compression in the lower back can cause pain and tightness that radiates down the leg into the calf.
1.7. Improper Stretching
Stretching incorrectly can also lead to tight calves. When stretches are performed too quickly, forcefully, or without proper technique, they can cause muscle strain and tightness.
- Ballistic Stretching: Rapid, bouncing movements during stretching can cause muscle tears and tightness.
- Insufficient Warm-Up: Stretching cold muscles can increase the risk of injury and tightness.
- Holding Stretches Too Briefly: Not holding stretches long enough can limit their effectiveness in lengthening muscle fibers.
2. Common Symptoms Associated with Tight Calves
Recognizing the symptoms of tight calves is essential for early intervention and effective management. These symptoms can range from mild discomfort to severe pain, impacting daily activities and overall quality of life.
2.1. Muscle Stiffness
Muscle stiffness is a primary symptom of tight calves. The calf muscles may feel rigid and resistant to movement, particularly after periods of rest or inactivity.
- Morning Stiffness: Calf stiffness is often more pronounced in the morning, gradually improving with movement.
- Post-Exercise Stiffness: Stiffness may also worsen after physical activity, indicating muscle fatigue and overuse.
- Limited Range of Motion: Stiffness can restrict ankle and foot movement, making it difficult to perform certain exercises or activities.
2.2. Pain and Discomfort
Pain and discomfort are common complaints associated with tight calves. The pain may range from a dull ache to sharp, shooting sensations, depending on the severity of the tightness.
- Localized Pain: Pain is typically felt in the calf muscles, often near the back of the lower leg.
- Referred Pain: In some cases, pain may radiate to the ankle, foot, or even the back of the thigh.
- Exacerbated Pain: Pain may worsen with activities that strain the calf muscles, such as walking, running, or standing.
2.3. Cramping
Muscle cramping is a sudden, involuntary contraction of the calf muscles, resulting in intense pain and temporary immobility. Cramps are often triggered by dehydration, electrolyte imbalances, or muscle fatigue.
- Nocturnal Cramps: Calf cramps are common at night, disrupting sleep and causing significant discomfort.
- Exercise-Induced Cramps: Cramps may occur during or after physical activity, especially in hot or humid conditions.
- Prolonged Cramps: Cramps can last from a few seconds to several minutes, requiring immediate relief measures.
2.4. Limited Ankle Flexibility
Tight calves can restrict ankle flexibility, making it difficult to perform movements such as dorsiflexion (lifting the foot towards the shin) and plantarflexion (pointing the toes downward).
- Difficulty Squatting: Limited ankle flexibility can make it challenging to perform deep squats or lunges.
- Compromised Gait: Reduced ankle movement can alter gait patterns, increasing the risk of injury to the knees, hips, and lower back.
- Balance Issues: Ankle stiffness can affect balance and stability, particularly during activities that require quick changes in direction.
2.5. Tenderness to the Touch
The calf muscles may feel tender to the touch, indicating inflammation or muscle strain. Palpation (pressing on the muscles) can reveal areas of increased sensitivity and discomfort.
- Localized Tenderness: Tenderness is often concentrated in specific areas of the calf muscles, such as trigger points or knots.
- Widespread Tenderness: In more severe cases, tenderness may be diffuse, affecting the entire calf muscle group.
- Pain with Pressure: Applying pressure to the calf muscles can elicit pain, indicating underlying muscle injury or inflammation.
2.6. Altered Gait
Tight calves can lead to an altered gait, or walking pattern, as the body attempts to compensate for reduced flexibility and muscle imbalances.
- Limping: Severe calf tightness can cause a noticeable limp, indicating significant pain and functional impairment.
- Toe Walking: Individuals with tight calves may walk on their toes to avoid stretching the calf muscles, further exacerbating the condition.
- Reduced Stride Length: Calf tightness can limit stride length, resulting in a shorter, less efficient gait.
2.7. Foot and Ankle Problems
Tight calves can contribute to various foot and ankle problems, including plantar fasciitis, Achilles tendinitis, and ankle sprains. The increased tension and strain on the lower leg can disrupt biomechanics and increase the risk of injury.
- Plantar Fasciitis: Tight calves can increase tension on the plantar fascia, leading to inflammation and heel pain.
- Achilles Tendinitis: Restricted ankle flexibility can strain the Achilles tendon, causing pain and inflammation.
- Ankle Sprains: Calf tightness can compromise ankle stability, increasing the risk of sprains and other injuries.
 Calf Stretch Technique
Calf Stretch Technique
3. Simple Stretches and Exercises to Relieve Tight Calves
Fortunately, several simple stretches and exercises can effectively relieve tight calves and improve lower leg flexibility. Incorporating these techniques into your daily routine can help prevent muscle stiffness, reduce pain, and enhance overall mobility.
3.1. Standing Calf Stretch
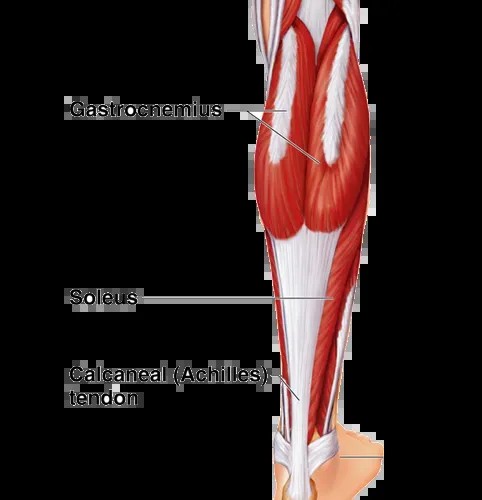
The standing calf stretch is a basic yet effective exercise for targeting the gastrocnemius, the larger of the two calf muscles. This stretch can be performed virtually anywhere and requires no special equipment.
- How to Perform:
- Stand facing a wall or sturdy object for support.
- Place your hands on the wall at shoulder height.
- Step one leg back, keeping the heel on the ground and the knee straight.
- Lean forward, feeling the stretch in the calf muscle of the back leg.
- Hold the stretch for 20-30 seconds.
- Repeat on the opposite leg.
- Benefits: Lengthens the gastrocnemius, improves ankle flexibility, and reduces muscle stiffness.
3.2. Soleus Stretch
The soleus stretch targets the soleus muscle, which lies beneath the gastrocnemius. This stretch is performed with a bent knee, allowing for a deeper stretch in the lower calf.
- How to Perform:
- Stand facing a wall or sturdy object for support.
- Place your hands on the wall at shoulder height.
- Step one leg back, bending the knee and keeping the heel on the ground.
- Lean forward, feeling the stretch in the lower calf muscle of the back leg.
- Hold the stretch for 20-30 seconds.
- Repeat on the opposite leg.
- Benefits: Lengthens the soleus, improves ankle flexibility, and helps alleviate tightness in the lower calf.
3.3. Towel Stretch
The towel stretch is a gentle exercise that can be performed while sitting, making it ideal for those with limited mobility or flexibility. This stretch helps to increase ankle range of motion and improve calf muscle length.
- How to Perform:
- Sit on the floor with your legs extended in front of you.
- Place a towel or resistance band around the ball of one foot.
- Gently pull back on the towel, keeping your knee straight.
- Hold the stretch for 20-30 seconds.
- Repeat on the opposite leg.
- Benefits: Increases ankle range of motion, stretches the calf muscles, and improves flexibility.
3.4. Calf Raises
Calf raises are a simple yet effective strengthening exercise for the calf muscles. This exercise helps to improve muscle strength, endurance, and overall lower leg function.
- How to Perform:
- Stand with your feet flat on the ground, shoulder-width apart.
- Slowly rise up onto the balls of your feet, lifting your heels off the ground.
- Hold the position for a second, then slowly lower your heels back to the ground.
- Repeat for 10-15 repetitions.
- Benefits: Strengthens the calf muscles, improves ankle stability, and enhances lower leg function.
3.5. Seated Calf Raises
Seated calf raises are a variation of the traditional calf raise that can be performed while sitting. This exercise is particularly beneficial for individuals with limited mobility or those who want to target the soleus muscle more specifically.
- How to Perform:
- Sit on a chair with your feet flat on the ground.
- Place your feet flat on the ground, shoulder-width apart.
- Slowly rise up onto the balls of your feet, lifting your heels off the ground.
- Hold the position for a second, then slowly lower your heels back to the ground.
- Repeat for 10-15 repetitions.
- Benefits: Strengthens the calf muscles, improves ankle stability, and enhances lower leg function.
3.6. Foam Rolling
Foam rolling is a self-massage technique that can help release tension and knots in the calf muscles. This technique involves using a foam roller to apply pressure to the muscles, promoting blood flow and reducing muscle stiffness.
- How to Perform:
- Sit on the floor with your legs extended in front of you.
- Place a foam roller under one calf.
- Use your hands to lift your hips off the ground.
- Roll the foam roller along your calf muscle, from the ankle to the knee.
- Repeat for 1-2 minutes, focusing on areas of tightness or discomfort.
- Repeat on the opposite leg.
- Benefits: Releases muscle tension, improves blood flow, reduces muscle stiffness, and enhances flexibility.
3.7. Dynamic Stretching
Dynamic stretching involves performing controlled movements that gradually increase range of motion and prepare the muscles for activity. Incorporating dynamic stretches into your warm-up routine can help prevent calf tightness and reduce the risk of injury.
- Examples of Dynamic Stretches:
- Ankle Circles: Rotate your ankles in both directions to improve flexibility and range of motion.
- Leg Swings: Swing your legs forward and backward to increase blood flow and prepare the calf muscles for activity.
- Toe Raises: Lift your toes off the ground while keeping your heels planted to activate the calf muscles and improve flexibility.
- Benefits: Improves flexibility, increases blood flow, prepares the muscles for activity, and reduces the risk of injury.
4. Home Remedies for Soothing Tight Calves
In addition to stretching and exercise, several home remedies can help soothe tight calves and provide relief from discomfort. These remedies are simple, cost-effective, and can be easily incorporated into your daily routine.
4.1. Heat Therapy
Applying heat to the calf muscles can help increase blood flow, relax muscle fibers, and reduce pain and stiffness. Heat therapy can be administered through various methods, including warm compresses, hot baths, and heating pads.
- Warm Compresses: Apply a warm, moist towel to the calf muscles for 15-20 minutes.
- Hot Baths: Soak in a warm bath with Epsom salts to help relax the muscles and reduce inflammation.
- Heating Pads: Use a heating pad on a low setting for 15-20 minutes at a time.
4.2. Cold Therapy
Cold therapy, or cryotherapy, can help reduce inflammation, numb pain, and alleviate muscle spasms. Applying cold packs or ice to the calf muscles can provide immediate relief from discomfort and promote healing.
- Ice Packs: Apply an ice pack wrapped in a towel to the calf muscles for 15-20 minutes at a time.
- Ice Massage: Gently massage the calf muscles with an ice cube for 5-10 minutes.
- Cold Compresses: Apply a cold, wet towel to the calf muscles for 15-20 minutes.
4.3. Massage Therapy
Massage therapy can help release muscle tension, improve blood flow, and reduce pain and stiffness in the calf muscles. Self-massage or professional massage can be beneficial for alleviating calf tightness and promoting relaxation.
- Self-Massage: Use your hands to gently massage the calf muscles, focusing on areas of tightness or discomfort.
- Professional Massage: Seek out a qualified massage therapist for a deep tissue or sports massage to help release muscle tension and improve flexibility.
4.4. Hydration
Staying adequately hydrated is essential for maintaining muscle function and flexibility. Dehydration can lead to muscle stiffness, cramping, and increased risk of injury. Aim to drink plenty of water throughout the day to keep your muscles hydrated and pliable.
- Drink Water Regularly: Aim to drink at least 8-10 glasses of water per day.
- Electrolyte Drinks: Consume electrolyte-rich beverages, such as sports drinks or coconut water, to help replenish essential minerals lost through sweat.
- Avoid Dehydrating Beverages: Limit your intake of caffeine and alcohol, as these can have a diuretic effect and contribute to dehydration.
4.5. Epsom Salt Soaks
Epsom salt soaks can help reduce muscle inflammation, relieve pain, and promote relaxation. Epsom salts contain magnesium, which is known for its muscle-relaxing properties. Soaking in a warm bath with Epsom salts can help soothe tight calves and improve overall comfort.
- How to Use:
- Fill a bathtub with warm water.
- Add 1-2 cups of Epsom salts to the water.
- Soak in the bath for 20-30 minutes.
- Gently massage the calf muscles while soaking to enhance relaxation.
4.6. Compression Therapy
Compression therapy involves wearing compression socks or sleeves to help improve blood flow, reduce swelling, and support the calf muscles. Compression garments can be particularly beneficial for athletes, individuals who stand for long periods, and those with circulatory issues.
- How to Use:
- Wear compression socks or sleeves during physical activity to help support the calf muscles and reduce fatigue.
- Wear compression garments after exercise to help reduce muscle soreness and promote recovery.
- Choose compression garments that provide a comfortable level of support without being too tight or restrictive.
4.7. Rest and Recovery
Allowing the calf muscles adequate rest and recovery is crucial for preventing overuse injuries and promoting healing. Avoid activities that exacerbate calf tightness and give your muscles time to repair and rebuild.
- Avoid Overexertion: Refrain from engaging in high-impact activities or exercises that strain the calf muscles until they have fully recovered.
- Get Adequate Sleep: Aim to get 7-8 hours of sleep per night to allow your body to repair and rejuvenate.
- Incorporate Rest Days: Include rest days in your exercise routine to give your muscles time to recover and rebuild.
5. How Your Diet Impacts Calf Health
Your diet plays a crucial role in muscle health, including the health of your calves. Consuming a balanced diet rich in essential nutrients can help support muscle function, reduce inflammation, and promote overall lower leg health.
5.1. Protein Intake
Protein is essential for muscle repair and growth. Adequate protein intake helps rebuild muscle fibers damaged during exercise and promotes muscle strength and flexibility.
- Recommended Intake: Aim to consume 0.8 grams of protein per kilogram of body weight per day.
- Good Sources of Protein: Lean meats, poultry, fish, eggs, dairy products, legumes, and nuts.
- Protein Supplements: Consider using protein supplements, such as whey protein or casein protein, to help meet your protein needs.
5.2. Hydration
As mentioned earlier, hydration is crucial for muscle function and flexibility. Dehydration can lead to muscle stiffness, cramping, and increased risk of injury.
- Drink Water Regularly: Aim to drink at least 8-10 glasses of water per day.
- Electrolyte Drinks: Consume electrolyte-rich beverages, such as sports drinks or coconut water, to help replenish essential minerals lost through sweat.
- Avoid Dehydrating Beverages: Limit your intake of caffeine and alcohol, as these can have a diuretic effect and contribute to dehydration.
5.3. Potassium
Potassium is an essential mineral that helps regulate muscle contractions and fluid balance. Potassium deficiency can lead to muscle cramping and weakness, contributing to calf tightness.
- Recommended Intake: Aim to consume 3,500-4,700 mg of potassium per day.
- Good Sources of Potassium: Bananas, oranges, potatoes, spinach, and avocados.
- Potassium Supplements: Consider using potassium supplements, but consult with a healthcare provider before starting any new supplement regimen.
5.4. Magnesium
Magnesium is another essential mineral that plays a crucial role in muscle function and relaxation. Magnesium deficiency can lead to muscle spasms, cramping, and increased muscle tension.
- Recommended Intake: Aim to consume 310-420 mg of magnesium per day.
- Good Sources of Magnesium: Dark leafy greens, nuts, seeds, whole grains, and legumes.
- Magnesium Supplements: Consider using magnesium supplements, such as magnesium citrate or magnesium glycinate, to help meet your magnesium needs.
5.5. Calcium
Calcium is essential for muscle contractions and nerve function. Adequate calcium intake helps ensure proper muscle function and reduces the risk of muscle cramping.
- Recommended Intake: Aim to consume 1,000-1,200 mg of calcium per day.
- Good Sources of Calcium: Dairy products, leafy green vegetables, fortified plant-based milks, and tofu.
- Calcium Supplements: Consider using calcium supplements, but consult with a healthcare provider before starting any new supplement regimen.
5.6. Anti-Inflammatory Foods
Consuming foods with anti-inflammatory properties can help reduce muscle inflammation, alleviate pain, and promote healing. Incorporating these foods into your diet can help soothe tight calves and improve overall muscle health.
- Foods with Anti-Inflammatory Properties: Fatty fish (salmon, mackerel), berries, cherries, turmeric, ginger, and green tea.
- Avoid Inflammatory Foods: Limit your intake of processed foods, sugary drinks, and unhealthy fats, as these can contribute to inflammation and muscle pain.
5.7. Vitamins
Certain vitamins, such as vitamin D and vitamin E, play a crucial role in muscle health and function. Vitamin D helps regulate calcium absorption and bone health, while vitamin E acts as an antioxidant, protecting muscle cells from damage.
- Vitamin D: Aim to get 600-800 IU of vitamin D per day through sunlight exposure, fortified foods, or supplements.
- Vitamin E: Aim to get 15 mg of vitamin E per day through nuts, seeds, vegetable oils, and leafy green vegetables.
6. When to Seek Professional Help for Tight Calves
While many cases of tight calves can be managed with self-care measures, it is essential to know when to seek professional help. Persistent or severe symptoms may indicate an underlying medical condition that requires medical attention.
6.1. Persistent Pain
If calf pain persists despite home remedies and self-care measures, it is essential to seek professional help. Persistent pain may indicate a more serious underlying condition that requires medical intervention.
- Chronic Pain: Pain that lasts for more than a few weeks may require medical evaluation.
- Unremitting Pain: Pain that does not improve with rest, stretching, or other self-care measures should be evaluated by a healthcare provider.
6.2. Severe Symptoms
Severe symptoms, such as intense pain, swelling, or difficulty walking, warrant immediate medical attention. These symptoms may indicate a serious injury or underlying medical condition that requires prompt treatment.
- Inability to Bear Weight: Difficulty or inability to put weight on the affected leg should be evaluated by a healthcare provider.
- Significant Swelling: Significant swelling or inflammation of the calf muscles may indicate a serious injury or infection.
6.3. Numbness or Tingling
Numbness or tingling in the calf, foot, or toes may indicate nerve compression or damage. These symptoms should be evaluated by a healthcare provider to determine the underlying cause and appropriate treatment.
- Nerve Compression: Conditions such as sciatica or peripheral neuropathy can cause numbness and tingling in the lower leg.
- Nerve Damage: Trauma or injury to the nerves in the calf can result in numbness and tingling.
6.4. Signs of Infection
Signs of infection, such as redness, warmth, or pus, may indicate a serious underlying condition that requires immediate medical attention. Seek medical care promptly if you suspect an infection.
- Redness: Redness or discoloration of the skin may indicate an infection.
- Warmth: Increased warmth or heat around the calf muscles may suggest an infection.
- Pus: Drainage of pus or other fluids from the affected area is a clear sign of infection.
6.5. Underlying Medical Conditions
If you have an underlying medical condition, such as diabetes, peripheral artery disease, or neuropathy, it is essential to seek professional help for tight calves. These conditions can complicate the management of calf tightness and may require specialized treatment.
- Diabetes: High blood sugar levels can damage nerves and blood vessels, affecting muscle function and requiring careful management.
- Peripheral Artery Disease: PAD reduces blood flow to the legs, causing muscle pain and tightness that requires medical intervention.
- Neuropathy: Nerve damage can cause pain, numbness, and tingling in the lower leg, requiring specialized treatment.
6.6. Lack of Improvement
If your symptoms do not improve with self-care measures and lifestyle modifications, it is important to seek professional help. A healthcare provider can evaluate your condition, diagnose any underlying issues, and recommend appropriate treatment strategies.
- Persistent Symptoms: If your symptoms persist despite home remedies and self-care measures, it is time to seek medical attention.
- Worsening Symptoms: If your symptoms worsen over time, it is essential to consult with a healthcare provider for further evaluation and treatment.
7. Preventing Tight Calves: Long-Term Strategies
Preventing tight calves involves adopting long-term strategies that promote muscle health, flexibility, and overall lower leg function. Incorporating these strategies into your daily routine can help reduce the risk of calf tightness and improve your overall quality of life.
7.1. Regular Stretching
Incorporating regular stretching into your daily routine is essential for maintaining muscle flexibility and preventing calf tightness. Aim to stretch your calf muscles at least 2-3 times per day to keep them pliable and reduce the risk of stiffness.
- Standing Calf Stretch: Perform the standing calf stretch to target the gastrocnemius muscle.
- Soleus Stretch: Perform the soleus stretch to target the soleus muscle.
- Towel Stretch: Use the towel stretch to improve ankle range of motion and stretch the calf muscles.
7.2. Consistent Exercise
Engaging in regular exercise can help improve muscle strength, endurance, and flexibility. Choose activities that promote lower leg health and avoid overuse injuries.
- Low-Impact Activities: Activities such as walking, swimming, and cycling are gentle on the calf muscles and promote cardiovascular health.
- Strength Training: Incorporate strength training exercises, such as calf raises and seated calf raises, to improve muscle strength and stability.
7.3. Proper Hydration
Maintaining adequate hydration is crucial for muscle function and flexibility. Aim to drink plenty of water throughout the day to keep your muscles hydrated and pliable.
- Drink Water Regularly: Aim to drink at least 8-10 glasses of water per day.
- Electrolyte Drinks: Consume electrolyte-rich beverages, such as sports drinks or coconut water, to help replenish essential minerals lost through sweat.
- Avoid Dehydrating Beverages: Limit your intake of caffeine and alcohol, as these can have a diuretic effect and contribute to dehydration.
7.4. Balanced Diet
Consuming a balanced diet rich in essential nutrients can help support muscle function, reduce inflammation, and promote overall lower leg health.
- Protein Intake: Consume adequate protein to support muscle repair and growth.
- Potassium Intake: Ensure adequate potassium intake to regulate muscle contractions and fluid balance.
- Magnesium Intake: Ensure adequate magnesium intake to promote muscle relaxation and reduce muscle tension.
7.5. Appropriate Footwear
Wearing appropriate footwear can help support proper foot and ankle alignment, reducing strain on the calf muscles. Choose shoes that provide adequate support and cushioning for your feet.
- Supportive Shoes: Wear shoes with good arch support and cushioning to reduce stress on the calf muscles.
- Avoid High Heels: Limit your use of high heels, as they can contribute to calf tightness and muscle imbalances.
- Replace Worn-Out Shoes: Replace worn-out shoes regularly to ensure they provide adequate support and cushioning.
7.6. Regular Breaks
Taking regular breaks during periods of prolonged sitting or standing can help prevent muscle stiffness and fatigue. Get up and move around every 30-60 minutes to keep your muscles active and pliable.
- Stretch Breaks: Incorporate calf stretches into your breaks to keep your muscles flexible and reduce the risk of stiffness.
- Walking Breaks: Take short walks to improve blood flow and keep your muscles active.
7.7. Gradual Progression
When starting a new exercise routine or increasing your activity level, it is important to progress gradually to avoid overuse injuries. Increase the intensity and duration of your workouts slowly to allow your muscles to adapt and avoid strain.
- Start Slowly: Begin with low-intensity exercises and gradually increase the intensity and duration of your workouts.
- Listen to Your Body: Pay attention to your body’s signals and avoid pushing yourself too hard, especially when starting a new exercise routine.
8. The Connection Between Tight Calves and Other Body Parts
Tight calves can have a ripple effect, impacting other parts of your body. Understanding these connections can help you address the root causes of calf tightness and prevent related issues.
8.1. Feet
Tight calves can contribute to various foot problems, including plantar fasciitis, heel pain, and bunions. The increased tension in the calf muscles can pull on the plantar fascia, the thick band of tissue that runs along the bottom of the foot, leading to inflammation and pain.
- Plantar Fasciitis: Tight calves can increase tension on the plantar fascia, causing inflammation and heel pain.
- Heel Pain: Tight calves can alter foot biomechanics, leading to increased stress on the heel and surrounding tissues.
- Bunions: Tight calves can contribute to abnormal foot mechanics, increasing the risk of bunion development.
8.2. Ankles
Tight calves can restrict ankle flexibility, increasing the risk of ankle sprains, Achilles tendinitis, and other ankle-related injuries. Restricted ankle movement can also affect gait patterns, increasing the risk of injury to the knees, hips, and lower back.
- Ankle Sprains: Tight calves can compromise ankle stability, increasing the risk of sprains and other injuries.
- Achilles Tendinitis: Restricted ankle flexibility can strain the Achilles tendon, causing pain and inflammation.
- Limited Range of Motion: Calf tightness can limit ankle movement, making it difficult to perform certain exercises or activities.
8.3. Knees
Tight calves can alter knee biomechanics, increasing the risk of knee pain, patellar tendinitis, and other knee-related issues. Restricted ankle flexibility can affect gait patterns, placing additional stress on the knees.
- Knee Pain: Tight calves can alter knee alignment and increase stress on the knee joint, leading to pain and discomfort.
- Patellar Tendinitis: Tight calves can contribute to patellar tendinitis, an inflammation of the tendon that connects the kneecap to the shinbone.
- Compensatory Movement: When the calves are tight, the body may compensate by altering the way the knees move, leading to increased wear and tear.
8.4. Hips
Tight calves can affect hip alignment and function, increasing the risk of hip pain, muscle imbalances, and other hip-related issues. Altered gait patterns resulting from tight calves can place additional stress on the hip joints.
- Hip Pain: Tight calves can alter hip alignment and increase stress on the hip joint, leading to pain and discomfort.
- Muscle Imbalances: Tight calves can contribute to muscle imbalances in the hips and lower back, increasing the risk of pain and injury.
- Gait Issues: Altered gait patterns resulting from tight calves can place additional stress on the hip joints.
8.5. Lower Back
Tight calves can contribute to lower back pain by altering posture and gait patterns. Muscle imbalances resulting from tight calves can place additional stress on the lower back, leading to pain and discomfort.
- Lower Back Pain: Tight calves can alter posture and gait patterns, increasing stress on the lower back and leading to pain.
- Muscle Imbalances: Tight calves can contribute to muscle imbalances in the lower back, increasing the risk of pain and injury.
- Compensatory Movement: When the calves are tight, the body may compensate by altering the way the back moves, leading to increased wear and tear.
8.6. Hamstrings
Tight calves are often associated with tight hamstrings. The hamstrings and calf muscles work together to control leg movement, and tightness in one area can affect the other.
- Muscle Chain: Tightness in the calf muscles can lead to increased tension in the hamstrings, and vice versa.
- Stretching: When stretching the hamstrings, it is also important to stretch the calves to maintain balance and flexibility.
9. Latest Research on Calf Muscle Tightness
Staying updated with the latest research on calf muscle tightness can provide valuable insights into effective prevention and treatment strategies. Scientific studies offer evidence-based recommendations for managing calf tightness and improving lower leg health.
9.1. The Role of Stretching in Calf Muscle Flexibility
A study published in the “Journal of Strength and Conditioning Research” examined the effects of static stretching on calf muscle flexibility. The study found that regular static stretching significantly improved calf muscle flexibility and range of motion.
- Study Findings: Static stretching, when performed consistently, can increase calf muscle length and reduce stiffness.
- Recommendations: Incorporate static stretching into your daily routine, holding each stretch for 20-30 seconds, to improve calf muscle flexibility.
9.2. The Impact of Foam Rolling on Muscle Recovery
Research published in the “Journal of Athletic Training” investigated the impact of foam rolling on muscle recovery after exercise. The study found that foam rolling can reduce muscle soreness, improve blood flow, and enhance muscle recovery.
- Study Findings: Foam rolling can help release muscle tension, improve blood flow, and reduce muscle stiffness.
- Recommendations: Use foam rolling after exercise to help reduce muscle soreness and promote recovery.
9.3. The Effect of Hydration on Muscle Cramping
A study published in the “Journal of the American College of Nutrition” examined the effect of hydration on muscle cramping during exercise. The study found that dehydration can increase the risk of muscle cramping and that adequate hydration is essential for preventing muscle cramps.
- Study Findings: Dehydration can lead to electrolyte imbalances and increase the risk of muscle cramping.
- Recommendations: Stay adequately hydrated by drinking plenty of water and electrolyte-rich beverages to prevent muscle cramps.
9.4. The Relationship Between Footwear and Calf Muscle Tightness
Research published in the “Journal of Foot and Ankle Research” investigated the relationship between footwear and calf muscle tightness. The study found that wearing high heels can contribute to calf muscle tightness and that switching to supportive footwear can help alleviate this issue.
- Study Findings: High heels can cause the calf muscles to shorten and tighten over time.
- Recommendations: Wear supportive shoes with good arch support and cushioning to reduce stress on the calf muscles.
9.5. The Role of Age in Calf Muscle Flexibility
A study published in the “Journal of Gerontology” examined the role of age in calf muscle flexibility. The study found that calf muscle flexibility decreases with age and that regular stretching and exercise can help maintain flexibility.
- Study Findings: Calf muscle flexibility decreases with age due to changes in muscle composition and elasticity.
- Recommendations: Incorporate regular stretching and exercise into your routine to maintain calf muscle flexibility as you age.
10. FAQ About Tight Calves
Here are some frequently asked questions about tight calves:
- What causes tight calves in the morning?
Tight calves in the morning are often due to inactivity during sleep, leading to decreased blood flow and muscle stiffness. - Can dehydration cause tight calves?
Yes, dehydration can lead to electrolyte imbalances and muscle stiffness, contributing to tight calves. - **How can I quickly