Are your period pains making you dread that time of the month? At WHY.EDU.VN, we understand how debilitating severe menstrual cramps can be, and we’re here to shed light on the potential causes and effective relief strategies. We aim to empower you with knowledge and solutions, helping you manage your monthly discomfort. Discover effective strategies for pain management, explore hormonal influences, and understand potential underlying causes.
1. Understanding Menstrual Cramps: What’s Normal and What’s Not
Menstrual cramps, also known as dysmenorrhea, are a common experience for many women during their periods. They occur when the uterus contracts to shed its lining, resulting in pain and discomfort in the lower abdomen. However, the intensity of these cramps can vary greatly from person to person. It’s essential to understand the difference between normal and severe period cramps to seek appropriate care and relief.
1.1. Defining Normal Period Cramps
Normal period cramps are typically mild to moderate in intensity and can be managed with over-the-counter pain relievers and home remedies. They usually start a day or two before your period and subside within the first few days of menstruation. Common symptoms of normal period cramps include:
- Aching or throbbing pain in the lower abdomen
- Pain that may radiate to the lower back and thighs
- Bloating
- Mild nausea
1.2. Recognizing Severe Period Cramps
Severe period cramps, on the other hand, are intense and debilitating, interfering with daily activities and quality of life. They may be accompanied by additional symptoms like:
- Excruciating pain in the lower abdomen
- Severe lower back pain
- Nausea and vomiting
- Diarrhea
- Headaches
- Dizziness
If you experience severe period cramps that significantly disrupt your life, it’s crucial to consult a healthcare professional for further evaluation and guidance.
1.3. Differentiating Between Primary and Secondary Dysmenorrhea
Dysmenorrhea is classified into two types: primary and secondary. Understanding the difference is key to identifying the underlying cause of your painful periods.
- Primary dysmenorrhea: This type occurs in women who have normal pelvic anatomy and is not caused by an underlying medical condition. It’s often related to hormonal imbalances and the production of prostaglandins, chemicals that cause the uterus to contract.
- Secondary dysmenorrhea: This type is caused by an underlying medical condition, such as endometriosis, fibroids, or pelvic inflammatory disease (PID). The pain associated with secondary dysmenorrhea tends to be more severe and may worsen over time.
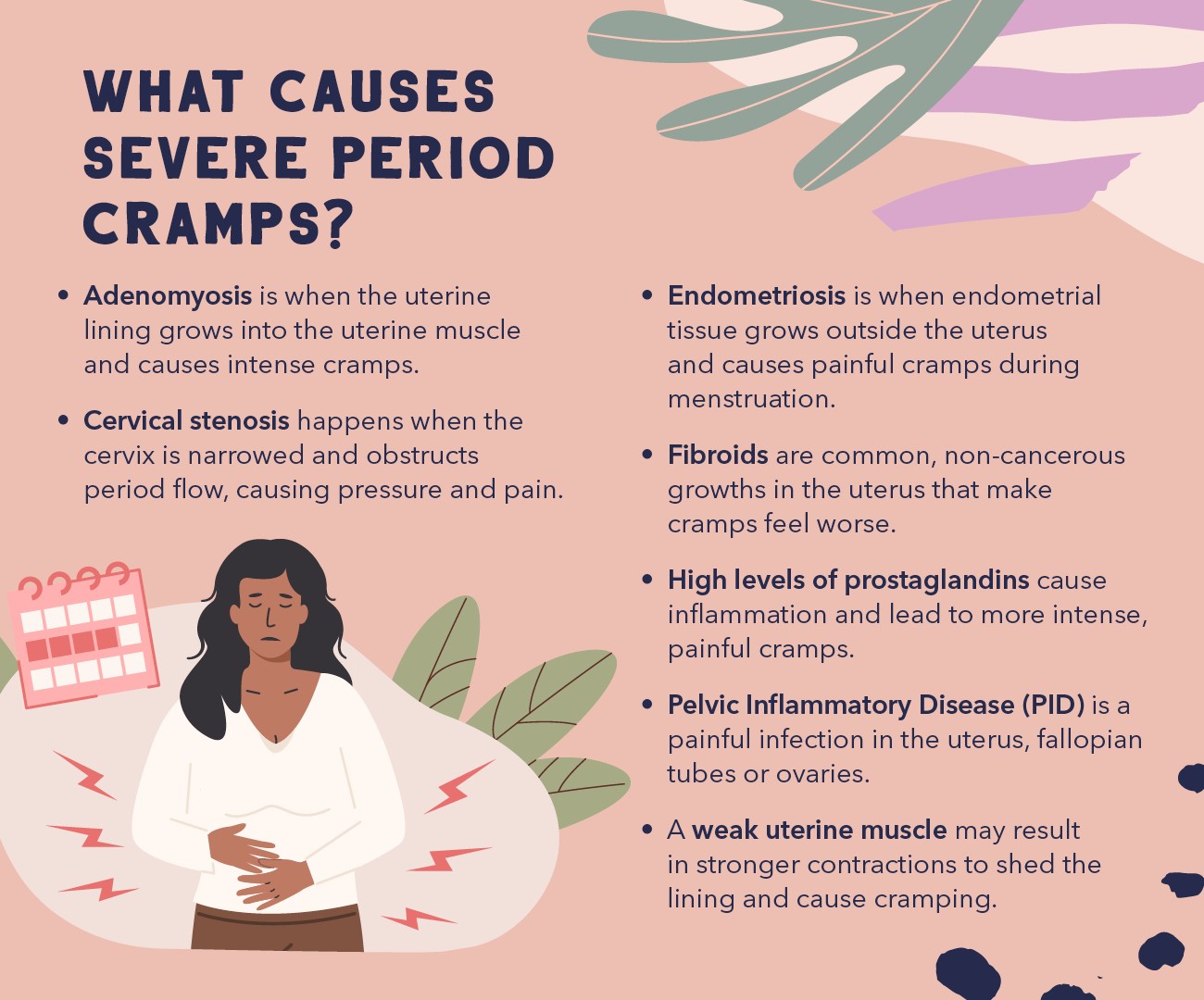
2. Exploring the Potential Causes of Intense Menstrual Cramps
Several factors can contribute to the intensity of menstrual cramps. Some of the most common causes include hormonal imbalances, underlying medical conditions, and lifestyle factors. Understanding these potential causes can help you identify the root of your painful periods and seek appropriate treatment.
2.1. Hormonal Imbalances and Prostaglandins
Hormones play a crucial role in regulating the menstrual cycle and can significantly impact the severity of period cramps. Prostaglandins, hormone-like substances, are released by the uterine lining during menstruation and cause the uterus to contract. Higher levels of prostaglandins are associated with more intense uterine contractions and, consequently, more severe pain.
- Prostaglandins and Inflammation: Prostaglandins also contribute to inflammation, further exacerbating period pain.
- Hormonal Contraceptives: Hormonal birth control methods, such as birth control pills, can help regulate hormone levels and reduce the production of prostaglandins, leading to milder menstrual cramps.
2.2. Underlying Medical Conditions
In some cases, severe period cramps may be a symptom of an underlying medical condition. Some of the most common conditions associated with painful periods include:
- Endometriosis: This condition occurs when the tissue that normally lines the uterus (endometrium) grows outside the uterus. This misplaced tissue can cause inflammation, scarring, and severe pain, especially during menstruation. According to the Endometriosis Association, endometriosis affects an estimated 1 in 10 women of reproductive age.
- Fibroids: These non-cancerous growths in the uterus can cause heavy bleeding, prolonged periods, and severe cramps. The size and location of fibroids can influence the intensity of period pain.
- Adenomyosis: This condition occurs when the endometrial tissue grows into the muscular wall of the uterus. It can cause the uterus to become enlarged and painful, leading to severe menstrual cramps.
- Pelvic Inflammatory Disease (PID): This infection of the reproductive organs can cause chronic pelvic pain, including severe period cramps. PID is often caused by sexually transmitted infections (STIs).
- Cervical Stenosis: A narrowing of the cervix can obstruct menstrual flow, leading to increased pressure and pain.
- Ovarian Cysts: While most ovarian cysts are harmless, some can cause pelvic pain and contribute to more painful periods.
2.3. Lifestyle Factors
Certain lifestyle factors can also influence the severity of menstrual cramps. These include:
- Diet: A diet high in processed foods, sugar, and unhealthy fats can contribute to inflammation and worsen period pain.
- Lack of Exercise: Regular physical activity can help reduce inflammation and improve blood flow, potentially easing menstrual cramps.
- Stress: High levels of stress can exacerbate pain and discomfort, including period cramps.
- Smoking: Smoking can constrict blood vessels and reduce blood flow to the uterus, potentially worsening menstrual cramps.
3. Symptoms Associated with Severe Menstrual Cramps
Severe period cramps can manifest in various ways, affecting not only the lower abdomen but also other parts of the body. Recognizing these symptoms can help you better understand your experience and communicate it effectively to your healthcare provider.
3.1. Physical Symptoms
The most common physical symptoms associated with severe menstrual cramps include:
- Intense lower abdominal pain: This is the hallmark symptom of dysmenorrhea and can range from a constant ache to sharp, stabbing pains.
- Lower back pain: Pain often radiates to the lower back, causing stiffness and discomfort.
- Thigh pain: Some women experience pain in their thighs, which may be caused by referred pain from the uterus.
- Nausea and vomiting: Severe pain can trigger nausea and vomiting in some individuals.
- Diarrhea: Changes in hormone levels during menstruation can affect bowel function, leading to diarrhea.
- Headaches: Hormonal fluctuations can also trigger headaches or migraines.
- Fatigue: The combination of pain, discomfort, and hormonal changes can lead to fatigue and exhaustion.
3.2. Emotional and Psychological Symptoms
Severe period cramps can also have a significant impact on emotional and psychological well-being. Common symptoms include:
- Irritability: Hormonal changes can make you feel more irritable and easily frustrated.
- Anxiety: The anticipation of painful periods can lead to anxiety and worry.
- Depression: Some women experience symptoms of depression, such as sadness, hopelessness, and loss of interest in activities.
- Difficulty concentrating: Pain and discomfort can make it difficult to focus and concentrate on tasks.
- Sleep disturbances: Severe cramps can disrupt sleep, leading to insomnia or restless sleep.
3.3. When to Seek Medical Attention
It’s crucial to seek medical attention if you experience any of the following symptoms in addition to severe period cramps:
- Heavy bleeding: Soaking through a pad or tampon every hour for several consecutive hours.
- Passing large blood clots: This may indicate an underlying condition like fibroids.
- Pain between periods: This could be a sign of endometriosis or another pelvic condition.
- Fever: This may indicate an infection, such as pelvic inflammatory disease (PID).
- Sudden, severe pain: This could be a sign of a ruptured ovarian cyst or another emergency.
4. Effective Strategies for Relieving Painful Menstrual Cramps
Fortunately, various strategies can help alleviate the pain and discomfort associated with severe menstrual cramps. These include over-the-counter pain relievers, prescription medications, home remedies, and lifestyle changes.
4.1. Over-the-Counter Pain Relievers
Over-the-counter pain relievers are often the first line of defense against menstrual cramps. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen are particularly effective because they reduce the production of prostaglandins.
- Ibuprofen: A common and effective NSAID for relieving menstrual cramps. Follow the dosage instructions on the label.
- Naproxen: Another NSAID that can provide longer-lasting pain relief than ibuprofen.
- Acetaminophen: While not an NSAID, acetaminophen can also help alleviate pain associated with menstrual cramps.
4.2. Prescription Medications
In some cases, over-the-counter pain relievers may not be enough to manage severe period cramps. Your doctor may prescribe stronger pain medications or other treatments, such as:
- Hormonal birth control: Birth control pills, patches, or rings can help regulate hormone levels and reduce the severity of menstrual cramps.
- Hormonal IUD: An intrauterine device (IUD) that releases progestin can also help reduce menstrual pain and bleeding.
- Gonadotropin-releasing hormone (GnRH) agonists: These medications can temporarily stop the production of estrogen, which can help shrink fibroids and reduce pain.
- Surgery: In severe cases, surgery may be necessary to remove fibroids, endometrial tissue, or other underlying causes of painful periods.
4.3. Home Remedies and Lifestyle Changes
In addition to medications, several home remedies and lifestyle changes can help alleviate menstrual cramps:
- Heat therapy: Applying a heating pad or taking a warm bath can help relax muscles and ease pain. A study published in the “Journal of Alternative and Complementary Medicine” found that heat therapy was as effective as ibuprofen in relieving menstrual cramps.
- Exercise: Regular physical activity can help reduce inflammation and improve blood flow, potentially easing menstrual cramps.
- Diet: Eating a healthy diet rich in fruits, vegetables, and whole grains can help reduce inflammation and improve overall health.
- Stress management: Practicing stress-reducing techniques like yoga, meditation, or deep breathing can help alleviate pain and discomfort.
- Herbal remedies: Some herbal remedies, such as ginger, chamomile, and peppermint, have been shown to have anti-inflammatory and pain-relieving properties.
- Acupuncture: This traditional Chinese medicine technique involves inserting thin needles into specific points on the body to relieve pain and promote healing. A review of studies published in the “American Journal of Obstetrics and Gynecology” found that acupuncture may be effective in reducing menstrual pain.
4.4. Complementary and Alternative Therapies
Beyond conventional medical treatments and home remedies, some women find relief from menstrual cramps through complementary and alternative therapies. These approaches may include:
- Acupressure: Similar to acupuncture, acupressure involves applying pressure to specific points on the body to relieve pain and promote relaxation.
- Massage: Massaging the lower abdomen and back can help relax muscles and ease pain.
- Yoga: Certain yoga poses can help stretch and strengthen the muscles in the pelvic area, potentially reducing menstrual cramps.
- Transcutaneous Electrical Nerve Stimulation (TENS): This therapy involves using a small device to deliver electrical impulses to the skin, which can help block pain signals.
5. The Role of Diet and Nutrition in Managing Menstrual Cramps
What you eat can significantly impact the severity of your menstrual cramps. A healthy, balanced diet can help reduce inflammation, regulate hormone levels, and provide essential nutrients that support overall health and well-being.
5.1. Foods to Emphasize
Focus on incorporating these foods into your diet to help ease menstrual cramps:
- Fruits and vegetables: These are rich in antioxidants and anti-inflammatory compounds.
- Whole grains: These provide fiber and essential nutrients.
- Lean protein: This helps stabilize blood sugar levels and reduce cravings.
- Healthy fats: Omega-3 fatty acids, found in fatty fish, flaxseeds, and walnuts, can help reduce inflammation.
- Calcium-rich foods: Calcium can help relax muscles and ease cramps. Good sources include dairy products, leafy green vegetables, and fortified foods.
- Magnesium-rich foods: Magnesium can also help relax muscles and reduce pain. Good sources include dark chocolate, nuts, seeds, and whole grains.
- Iron-rich foods: Iron is essential for preventing anemia, which can worsen menstrual cramps. Good sources include red meat, poultry, beans, and leafy green vegetables.
- Hydration: Staying hydrated is crucial for overall health and can help reduce bloating and discomfort.
5.2. Foods to Avoid or Limit
Limit or avoid these foods, as they can contribute to inflammation and worsen menstrual cramps:
- Processed foods: These are often high in sugar, unhealthy fats, and sodium, which can contribute to inflammation.
- Sugary drinks: These can cause blood sugar spikes and crashes, leading to increased cravings and inflammation.
- Caffeine: Caffeine can constrict blood vessels and worsen pain.
- Alcohol: Alcohol can dehydrate the body and worsen inflammation.
- Salty foods: These can contribute to bloating and water retention.
- Red meat: High consumption of red meat has been linked to increased inflammation.
5.3. Specific Nutrients and Supplements
Certain nutrients and supplements may be particularly helpful in managing menstrual cramps:
- Vitamin D: Vitamin D deficiency has been linked to increased pain sensitivity.
- Vitamin E: This antioxidant can help reduce inflammation and pain.
- Omega-3 fatty acids: These can help reduce inflammation and pain.
- Magnesium: This mineral can help relax muscles and ease cramps.
- Calcium: This mineral can help relax muscles and ease cramps.
- Ginger: This herb has anti-inflammatory and pain-relieving properties.
- Turmeric: This spice contains curcumin, a potent anti-inflammatory compound.
6. Medical Conditions That Can Cause or Worsen Menstrual Cramps
As mentioned earlier, several underlying medical conditions can cause or worsen menstrual cramps. It’s essential to be aware of these conditions and seek medical attention if you suspect you may have one.
6.1. Endometriosis
Endometriosis is a chronic condition in which the tissue that normally lines the uterus grows outside the uterus. This misplaced tissue can cause inflammation, scarring, and severe pain, especially during menstruation.
- Symptoms: Severe menstrual cramps, pelvic pain, pain during intercourse, infertility, fatigue, and digestive problems.
- Diagnosis: Laparoscopy, a surgical procedure in which a small incision is made in the abdomen to visualize the pelvic organs.
- Treatment: Pain relievers, hormonal birth control, surgery to remove endometrial tissue, and fertility treatments.
6.2. Fibroids
Fibroids are non-cancerous growths in the uterus that can cause heavy bleeding, prolonged periods, and severe cramps.
- Symptoms: Heavy bleeding, prolonged periods, pelvic pain, frequent urination, constipation, and back pain.
- Diagnosis: Pelvic exam, ultrasound, MRI, and hysteroscopy.
- Treatment: Pain relievers, hormonal birth control, GnRH agonists, surgery to remove fibroids, and uterine artery embolization.
6.3. Adenomyosis
Adenomyosis occurs when the endometrial tissue grows into the muscular wall of the uterus. It can cause the uterus to become enlarged and painful, leading to severe menstrual cramps.
- Symptoms: Severe menstrual cramps, heavy bleeding, prolonged periods, pelvic pain, and an enlarged uterus.
- Diagnosis: Pelvic exam, ultrasound, MRI, and endometrial biopsy.
- Treatment: Pain relievers, hormonal birth control, GnRH agonists, and hysterectomy.
6.4. Pelvic Inflammatory Disease (PID)
PID is an infection of the reproductive organs that can cause chronic pelvic pain, including severe period cramps.
- Symptoms: Pelvic pain, fever, abnormal vaginal discharge, pain during intercourse, and irregular periods.
- Diagnosis: Pelvic exam, blood tests, and cultures.
- Treatment: Antibiotics.
6.5. Ovarian Cysts
While most ovarian cysts are harmless, some can cause pelvic pain and contribute to more painful periods.
- Symptoms: Pelvic pain, bloating, nausea, vomiting, and irregular periods.
- Diagnosis: Pelvic exam, ultrasound, and CT scan.
- Treatment: Pain relievers, hormonal birth control, and surgery to remove the cyst.
7. Navigating Diagnosis and Treatment Options for Severe Cramps
If you are experiencing severe menstrual cramps, seeking a proper diagnosis is the first step toward finding effective relief. Your healthcare provider will conduct a thorough evaluation to determine the underlying cause of your pain and recommend appropriate treatment options.
7.1. Diagnostic Procedures
Several diagnostic procedures may be used to evaluate severe menstrual cramps, including:
- Pelvic Exam: A physical examination of the reproductive organs to check for abnormalities.
- Ultrasound: A non-invasive imaging technique that uses sound waves to create images of the uterus, ovaries, and other pelvic structures.
- MRI: A more detailed imaging technique that uses magnetic fields and radio waves to create images of the pelvic organs.
- Hysteroscopy: A procedure in which a thin, lighted tube is inserted into the uterus to visualize the uterine lining.
- Laparoscopy: A surgical procedure in which a small incision is made in the abdomen to visualize the pelvic organs and obtain tissue samples for biopsy.
7.2. Treatment Approaches
The treatment approach for severe menstrual cramps will depend on the underlying cause and the severity of your symptoms. Common treatment options include:
- Pain Relievers: Over-the-counter or prescription pain relievers to manage pain.
- Hormonal Birth Control: Hormonal contraception to regulate hormone levels and reduce menstrual pain.
- Surgery: Surgical procedures to remove fibroids, endometrial tissue, or other abnormalities.
- Lifestyle Modifications: Dietary changes, exercise, and stress management techniques to improve overall health and reduce pain.
- Alternative Therapies: Acupuncture, massage, and other alternative therapies to complement conventional medical treatments.
8. The Psychological Impact of Severe Menstrual Cramps
It’s crucial to acknowledge the significant psychological impact that severe menstrual cramps can have on a woman’s life. The chronic pain and discomfort can lead to:
- Anxiety: The anticipation of painful periods can trigger anxiety and worry.
- Depression: The constant pain and disruption to daily life can contribute to feelings of sadness, hopelessness, and isolation.
- Irritability: Hormonal fluctuations and pain can make you feel more irritable and easily frustrated.
- Social Isolation: The inability to participate in social activities due to pain can lead to feelings of loneliness and isolation.
- Reduced Productivity: Pain and discomfort can make it difficult to focus and concentrate on work or school tasks.
It’s essential to seek support from healthcare professionals, therapists, or support groups to address the psychological impact of severe menstrual cramps.
9. The Future of Menstrual Cramp Research and Treatment
Research into menstrual cramps is ongoing, and new treatments are constantly being developed. Some promising areas of research include:
- Targeted Pain Medications: Developing pain medications that specifically target the pain pathways involved in menstrual cramps.
- Non-Hormonal Treatments: Exploring non-hormonal treatments for endometriosis and other conditions that cause severe menstrual cramps.
- Personalized Medicine: Tailoring treatment plans to individual needs based on genetic factors and other characteristics.
- Improved Diagnostic Tools: Developing more accurate and less invasive diagnostic tools for endometriosis and other pelvic conditions.
10. Addressing Common Myths and Misconceptions About Menstrual Cramps
Many myths and misconceptions surround menstrual cramps, which can prevent women from seeking appropriate care and relief. Let’s debunk some of the most common ones:
- Myth: Menstrual cramps are “all in your head.”
- Fact: Menstrual cramps are a real physical experience caused by uterine contractions and inflammation.
- Myth: You just have to “deal with” menstrual cramps.
- Fact: There are many effective treatments available for menstrual cramps, and you don’t have to suffer in silence.
- Myth: Exercise makes menstrual cramps worse.
- Fact: Regular exercise can help reduce inflammation and improve blood flow, potentially easing menstrual cramps.
- Myth: Only “weak” women experience severe menstrual cramps.
- Fact: Severe menstrual cramps can affect any woman, regardless of her physical or emotional strength.
- Myth: If your mother had bad menstrual cramps, you will too.
- Fact: While genetics can play a role in menstrual cramps, other factors, such as lifestyle and underlying medical conditions, also contribute.
It’s important to understand the truth about period pain and seek support.
Are you struggling to find reliable answers to your health questions? Do you feel overwhelmed by the abundance of information available online? At WHY.EDU.VN, we understand your challenges and offer a solution. Our website provides expert-backed information and a platform for you to ask your burning questions and receive personalized answers from specialists. Don’t let uncertainty hold you back – visit WHY.EDU.VN today and experience the peace of mind that comes with reliable, expert-driven answers. Contact us at 101 Curiosity Lane, Answer Town, CA 90210, United States. Whatsapp: +1 (213) 555-0101. Website: why.edu.vn.
FAQ: Understanding Your Period Pain
Here are some frequently asked questions about menstrual cramps:
- Is it normal to have severe menstrual cramps?
- While some discomfort during menstruation is common, severe cramps that disrupt your daily life are not normal and should be evaluated by a healthcare provider.
- What are the main causes of painful periods?
- Common causes include hormonal imbalances, endometriosis, fibroids, adenomyosis, and pelvic inflammatory disease.
- Can diet affect menstrual cramps?
- Yes, a healthy diet rich in fruits, vegetables, whole grains, and lean protein can help reduce inflammation and ease menstrual cramps.
- Are there any home remedies that can relieve period cramps?
- Yes, heat therapy, exercise, stress management, and herbal remedies like ginger and chamomile can help alleviate pain.
- When should I see a doctor for menstrual cramps?
- See a doctor if you experience severe cramps that disrupt your daily life, heavy bleeding, pain between periods, or other concerning symptoms.
- How are severe menstrual cramps diagnosed?
- Diagnosis may involve a pelvic exam, ultrasound, MRI, hysteroscopy, or laparoscopy.
- What are the treatment options for severe menstrual cramps?
- Treatment options include pain relievers, hormonal birth control, surgery, lifestyle modifications, and alternative therapies.
- Can stress worsen menstrual cramps?
- Yes, high levels of stress can exacerbate pain and discomfort.
- Is there a cure for endometriosis?
- Currently, there is no cure for endometriosis, but treatments can help manage the symptoms and improve quality of life.
- Can birth control help with menstrual cramps?
- Yes, hormonal birth control can help regulate hormone levels and reduce the severity of menstrual cramps.