Why Would A Urologist Do A Cystoscopy? This procedure, involving a cystoscope, is crucial for diagnosing and treating bladder and urethra issues. At WHY.EDU.VN, we provide comprehensive insights into cystoscopy indications, helping you understand when it’s necessary and what to expect. Explore bladder health, urinary tract health, and urological evaluations through our expert articles.
1. Understanding Cystoscopy: A Urologist’s Perspective
Cystoscopy is a medical procedure that allows a urologist to visualize the inside of the bladder and urethra. It involves inserting a thin, flexible or rigid tube with a camera and light source (cystoscope) into the urethra and advancing it into the bladder. This procedure is essential for diagnosing, monitoring, and treating various urinary tract conditions.
1.1 What is a Cystoscope?
A cystoscope is a specialized medical instrument used in cystoscopy. It consists of a thin tube, which can be either flexible or rigid, with a light source and a camera at the end. The camera transmits images to a monitor, allowing the urologist to see the lining of the urethra and bladder. Cystoscopes can also be equipped with additional tools for taking biopsies, removing stones, or performing other therapeutic procedures.
1.2 Types of Cystoscopy
There are two main types of cystoscopy: flexible and rigid.
- Flexible Cystoscopy: This type uses a flexible cystoscope, which is more comfortable for the patient. It is typically used for diagnostic purposes and minor procedures.
- Rigid Cystoscopy: This type uses a rigid cystoscope, which provides a clearer view and allows for more complex procedures, such as tumor removal or stone extraction.
2. Key Reasons for a Urologist to Perform a Cystoscopy
A urologist may recommend a cystoscopy for several reasons, including diagnosing urinary tract conditions, monitoring existing issues, and performing therapeutic interventions.
2.1 Diagnosing Urinary Tract Conditions
One of the primary reasons for performing a cystoscopy is to diagnose various conditions affecting the bladder and urethra.
2.1.1 Hematuria (Blood in Urine)
Hematuria, or blood in the urine, can be a sign of various underlying issues, ranging from minor infections to more serious conditions like bladder cancer.
Diagnostic Steps for Hematuria
| Step | Description |
|---|---|
| Urine Test | Initial test to confirm the presence of blood and rule out infection. |
| Cystoscopy | Visual examination of the bladder and urethra to identify the source of bleeding. |
| Imaging | CT scan or MRI to evaluate the kidneys and ureters. |
2.1.2 Urinary Tract Infections (UTIs)
Recurrent UTIs, especially in men, may warrant a cystoscopy to identify structural abnormalities or other underlying causes.
Common Causes of Recurrent UTIs
- Bladder stones
- Urethral strictures
- Enlarged prostate
- Bladder diverticula
2.1.3 Bladder Pain and Irritation
Chronic bladder pain and irritation, such as that experienced in interstitial cystitis (IC), can be evaluated using cystoscopy to rule out other conditions and assess the bladder lining.
Symptoms of Interstitial Cystitis
- Frequent urination
- Urgency
- Pelvic pain
- Painful urination
2.1.4 Urinary Incontinence and Overactive Bladder (OAB)
Cystoscopy can help determine the causes of urinary incontinence and OAB by identifying bladder abnormalities or neurological issues.
Possible Findings During Cystoscopy for Incontinence
- Bladder tumors
- Bladder stones
- Urethral strictures
- Inflammation
2.2 Monitoring Existing Conditions
Cystoscopy is also used to monitor the progression or recurrence of certain urinary tract conditions.
2.2.1 Bladder Cancer
Patients with a history of bladder cancer require regular cystoscopies to monitor for recurrence. This is a critical part of their follow-up care.
Frequency of Cystoscopy for Bladder Cancer Monitoring
| Stage of Cancer | Frequency of Cystoscopy |
|---|---|
| Low-risk | Every 3-6 months for the first 2 years, then annually. |
| High-risk | Every 3 months for the first 2 years, then every 6 months for the next 3 years, then annually. |
2.2.2 Urethral Strictures
Urethral strictures, or narrowing of the urethra, can be monitored using cystoscopy to assess the severity and guide treatment decisions.
Symptoms of Urethral Strictures
- Weak urine stream
- Straining to urinate
- Frequent UTIs
- Painful urination
2.3 Performing Therapeutic Interventions
In addition to diagnosis and monitoring, cystoscopy allows urologists to perform various therapeutic procedures.
2.3.1 Bladder Tumor Resection
Small bladder tumors can be removed during cystoscopy using a technique called transurethral resection of bladder tumor (TURBT).
Steps in TURBT
- Insertion of cystoscope into the bladder
- Identification of the tumor
- Resection of the tumor using a wire loop
- Cauterization of the tumor base to prevent bleeding
2.3.2 Bladder Stone Removal
Bladder stones can be fragmented and removed using specialized instruments passed through the cystoscope.
Methods of Bladder Stone Removal
- Cystolitholapaxy: Crushing the stone into smaller pieces and removing them.
- Laser Lithotripsy: Using a laser to break the stone into smaller fragments.
2.3.3 Urethral Stricture Treatment
Urethral strictures can be treated by dilating the urethra or performing a urethrotomy (incision of the stricture) using instruments passed through the cystoscope.
Types of Urethral Stricture Treatment
- Urethral Dilation: Stretching the urethra with progressively larger dilators.
- Direct Vision Internal Urethrotomy (DVIU): Incising the stricture under direct vision.
3. The Cystoscopy Procedure: What to Expect
Understanding the cystoscopy procedure can help alleviate anxiety and prepare patients for what to expect.
3.1 Pre-Procedure Preparation
Before undergoing a cystoscopy, patients may need to follow certain preparation guidelines.
Pre-Procedure Instructions
- Fasting: Depending on the type of anesthesia, patients may need to fast for several hours before the procedure.
- Medications: Patients should inform their urologist about all medications they are taking, as some may need to be temporarily discontinued.
- Antibiotics: In some cases, antibiotics may be prescribed to prevent infection.
3.2 During the Procedure
The cystoscopy procedure typically follows these steps:
-
Positioning: The patient lies on their back on an examination table, usually with their feet in stirrups.
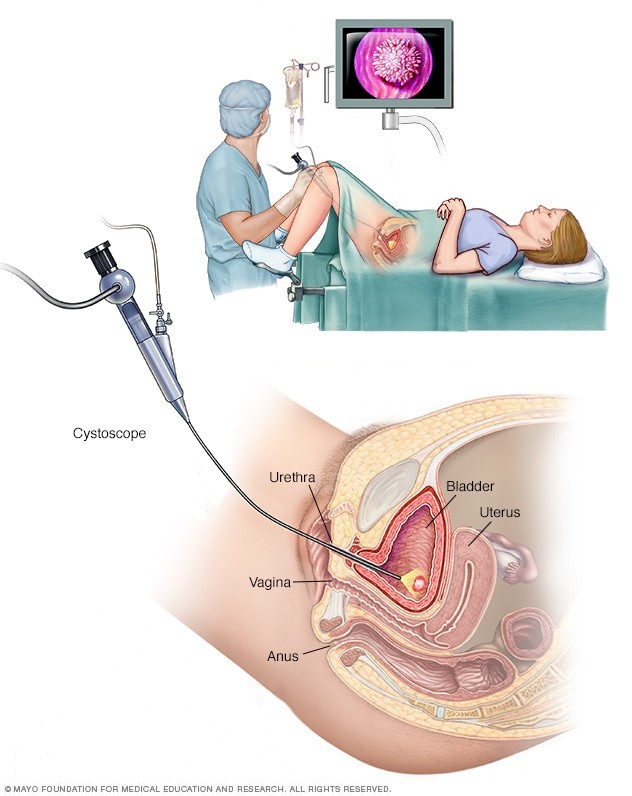 Patient positioning for cystoscopy
Patient positioning for cystoscopy -
Anesthesia: Local, regional, or general anesthesia may be used, depending on the complexity of the procedure and the patient’s comfort level.
-
Insertion: The urologist inserts the cystoscope into the urethra and gently advances it into the bladder.
-
Examination: The bladder is filled with sterile saline to improve visualization. The urologist examines the lining of the urethra and bladder for any abnormalities.
-
Intervention: If necessary, the urologist may perform biopsies, remove stones, or treat strictures during the procedure.
-
Removal: The cystoscope is carefully removed once the examination or intervention is complete.
3.3 Post-Procedure Care
After a cystoscopy, patients can expect some mild discomfort and should follow specific post-procedure care instructions.
Post-Procedure Instructions
- Hydration: Drink plenty of fluids to flush out the urinary tract.
- Pain Relief: Over-the-counter pain relievers can help alleviate discomfort.
- Monitoring: Watch for signs of infection, such as fever, chills, or increased pain.
- Activity: Avoid strenuous activities for a few days.
4. Potential Risks and Complications of Cystoscopy
While cystoscopy is generally a safe procedure, it is associated with some potential risks and complications.
4.1 Common Risks
- Urinary Tract Infection (UTI): The introduction of instruments into the urinary tract can increase the risk of infection.
- Bleeding: Minor bleeding is common after cystoscopy, especially if biopsies were taken.
- Pain and Discomfort: Patients may experience pain or discomfort during and after the procedure.
4.2 Rare Complications
- Bladder Perforation: In rare cases, the bladder wall can be perforated during cystoscopy.
- Urethral Injury: The urethra can be injured during the insertion of the cystoscope.
- Stricture Formation: Scar tissue can form in the urethra, leading to strictures.
4.3 Minimizing Risks
To minimize the risks associated with cystoscopy, urologists take several precautions.
Risk Minimization Strategies
- Sterile Technique: Using sterile instruments and techniques to prevent infection.
- Gentle Insertion: Carefully inserting the cystoscope to avoid injury.
- Appropriate Anesthesia: Providing adequate anesthesia to minimize pain and discomfort.
5. Alternative Procedures to Cystoscopy
In some cases, alternative procedures may be considered instead of cystoscopy.
5.1 Non-Invasive Imaging
Non-invasive imaging techniques, such as ultrasound, CT scans, and MRI, can provide valuable information about the urinary tract without the need for invasive procedures.
Advantages of Non-Invasive Imaging
- No risk of infection
- No need for anesthesia
- Less discomfort for the patient
5.2 Ureteroscopy
Ureteroscopy is a similar procedure to cystoscopy, but it involves examining the ureters (the tubes that carry urine from the kidneys to the bladder) rather than the bladder itself.
Indications for Ureteroscopy
- Ureteral stones
- Ureteral tumors
- Ureteral strictures
5.3 Bladder Biopsy (through other means)
In certain situations, a bladder biopsy may be obtained through other means, such as a percutaneous approach.
Percutaneous Bladder Biopsy
- A needle is inserted through the skin into the bladder to obtain a tissue sample.
- This approach is less common than cystoscopy with biopsy.
6. Understanding the Results of a Cystoscopy
The results of a cystoscopy can provide valuable information about the health of the urinary tract.
6.1 Normal Findings
Normal findings during a cystoscopy include a healthy-looking bladder and urethra, with no signs of tumors, stones, strictures, or inflammation.
6.2 Abnormal Findings
Abnormal findings may include:
-
Tumors: Growths in the bladder or urethra.
-
Stones: Mineral deposits in the bladder.
-
Strictures: Narrowing of the urethra.
-
Inflammation: Redness and swelling of the bladder or urethra.
-
Diverticula: Pouches or sacs in the bladder wall.
6.3 Follow-Up
Based on the results of the cystoscopy, the urologist will recommend appropriate follow-up care, which may include further testing, treatment, or monitoring.
7. The Role of WHY.EDU.VN in Providing Urological Information
WHY.EDU.VN is dedicated to providing accurate, reliable, and comprehensive information about urological health. We aim to empower individuals to make informed decisions about their health by offering expert insights and resources.
7.1 Expert Content
Our content is developed by experienced healthcare professionals and urology experts who are committed to delivering evidence-based information.
7.2 Comprehensive Resources
We offer a wide range of resources, including articles, guides, and FAQs, covering various urological conditions and procedures.
7.3 Community Support
We foster a supportive community where individuals can ask questions, share experiences, and connect with others who have similar health concerns.
8. Case Studies: Real-Life Examples of Cystoscopy Use
To illustrate the practical application of cystoscopy, let’s examine a few real-life case studies.
8.1 Case Study 1: Diagnosing Bladder Cancer
A 65-year-old male presented with hematuria. A cystoscopy revealed a suspicious lesion in the bladder. A biopsy was performed during the cystoscopy, which confirmed the diagnosis of bladder cancer.
Treatment Plan
- TURBT to remove the tumor
- Intravesical chemotherapy to prevent recurrence
- Regular cystoscopy follow-up
8.2 Case Study 2: Managing Urethral Stricture
A 40-year-old male experienced difficulty urinating. A cystoscopy revealed a urethral stricture.
Treatment Plan
- Urethral dilation to widen the urethra
- Regular follow-up to monitor for recurrence
8.3 Case Study 3: Removing Bladder Stones
A 70-year-old female presented with recurrent UTIs. A cystoscopy revealed multiple bladder stones.
Treatment Plan
- Cystolitholapaxy to crush and remove the stones
- Antibiotics to treat the UTI
9. FAQ: Common Questions About Cystoscopy
Here are some frequently asked questions about cystoscopy to further clarify the procedure and its implications.
- Is cystoscopy painful? Most patients experience some discomfort during cystoscopy, but it is generally not very painful. Anesthesia can help minimize discomfort.
- How long does a cystoscopy take? A simple cystoscopy typically takes 5-15 minutes. More complex procedures may take longer.
- Can I eat before a cystoscopy? Depending on the type of anesthesia, you may need to fast for several hours before the procedure.
- What should I wear to a cystoscopy appointment? Wear comfortable, loose-fitting clothing.
- Can I drive myself home after a cystoscopy? If you receive sedation or general anesthesia, you will need someone to drive you home.
- When can I resume normal activities after a cystoscopy? Most patients can resume normal activities within a day or two.
- What are the signs of infection after a cystoscopy? Signs of infection include fever, chills, increased pain, and cloudy or bloody urine.
- How often should I have a cystoscopy if I have a history of bladder cancer? The frequency of cystoscopy depends on the stage and risk of recurrence. Your urologist will determine the appropriate schedule.
- Can a cystoscopy detect all types of bladder problems? Cystoscopy is effective for detecting many bladder problems, but some conditions may require additional testing.
- What if I’m anxious about having a cystoscopy? Talk to your urologist about your concerns. They can provide information and strategies to help you feel more comfortable.
10. The Future of Cystoscopy: Innovations and Advancements
The field of cystoscopy continues to evolve, with ongoing research and development aimed at improving the procedure and enhancing patient outcomes.
10.1 Enhanced Imaging Techniques
New imaging technologies, such as narrow-band imaging (NBI) and blue light cystoscopy, are being developed to improve the detection of bladder tumors.
Benefits of Enhanced Imaging
- Improved visualization of abnormal tissue
- Increased detection rates for bladder cancer
- Reduced risk of recurrence
10.2 Minimally Invasive Approaches
Researchers are exploring minimally invasive approaches to cystoscopy, such as using smaller and more flexible cystoscopes, to reduce patient discomfort and improve recovery times.
10.3 Artificial Intelligence (AI) Integration
AI is being integrated into cystoscopy to assist urologists in identifying and diagnosing bladder conditions.
AI Applications in Cystoscopy
- Automated image analysis
- Detection of subtle abnormalities
- Improved diagnostic accuracy
11. Conclusion: Empowering You with Knowledge About Cystoscopy
Understanding why a urologist might perform a cystoscopy is crucial for making informed decisions about your health. Cystoscopy is a valuable tool for diagnosing, monitoring, and treating various urinary tract conditions. At WHY.EDU.VN, we are committed to providing you with the knowledge and resources you need to navigate your urological health journey with confidence. Whether you’re dealing with hematuria, recurrent UTIs, bladder pain, or other urological concerns, understanding the role of cystoscopy can help you take proactive steps toward better health.
Do you have more questions about cystoscopy or other urological procedures? Visit why.edu.vn at 101 Curiosity Lane, Answer Town, CA 90210, United States, or contact us via Whatsapp at +1 (213) 555-0101 to get your questions answered by our team of experts. We’re here to provide the accurate, reliable information you need to make informed decisions about your health.