Dehydroepiandrosterone (DHEA) is a naturally occurring hormone in the human body that has garnered significant attention for its wide-ranging potential health benefits. Research spanning several decades suggests DHEA plays a crucial role in various physiological processes, from immune function to cognitive health. One intriguing aspect of DHEA is its secretion pattern, which naturally peaks at night. This raises a pertinent question: Why Take Dhea At Night? Understanding the science behind DHEA’s circadian rhythm and its potential benefits when taken in alignment with this natural pattern can offer valuable insights for those considering DHEA supplementation.
Understanding DHEA and Its Role in the Body
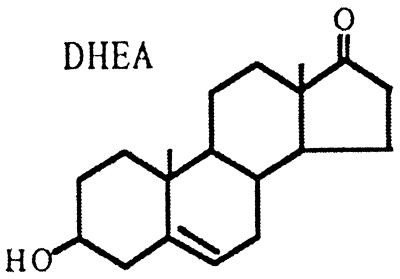
DHEA is a steroid hormone produced primarily by the adrenal glands. It serves as a precursor to both androgens and estrogens, the primary sex hormones in the body. While DHEA itself has mild androgenic effects, its conversion into more potent hormones like testosterone and estradiol in peripheral tissues contributes significantly to overall hormonal balance. This peripheral conversion is particularly important, as it allows for localized hormone action, minimizing systemic exposure and maximizing functional efficiency. It’s estimated that a substantial portion of sex hormones, particularly in men and postmenopausal women, originates from this peripheral DHEA conversion.
Beyond its role as a hormone precursor, DHEA has been implicated in a multitude of biological functions. Animal studies have suggested a wide array of potential benefits, including immuno-enhancement, anti-diabetic effects, anti-obesity properties, anticancer potential, neurotrophic effects, memory enhancement, and anti-aging properties. These findings have fueled interest in DHEA supplementation as a potential strategy to promote health and well-being, particularly in aging populations where DHEA levels naturally decline.
The Circadian Rhythm of DHEA Secretion
The human body operates on a 24-hour cycle known as the circadian rhythm, which governs various physiological processes, including hormone secretion. DHEA is no exception. The secretion of DHEA by the adrenal gland follows a pulsatile pattern, with a notable increase in frequency and amplitude during the night. This nocturnal surge in DHEA production is largely orchestrated by corticotropin (ACTH), a hormone released by the pituitary gland. ACTH stimulates the adrenal zona reticularis, the primary site of DHEA synthesis, leading to increased DHEA production and release into the bloodstream during the night.
This natural nighttime elevation of DHEA levels suggests a potential biological significance to this timing. While the precise reasons for this circadian rhythm are still being investigated, it’s hypothesized that this nocturnal surge may play a role in sleep regulation, cellular repair, and other nighttime physiological processes. Interestingly, while DHEA secretion exhibits this robust nocturnal pattern, cortisol, another adrenal hormone also regulated by ACTH, maintains its pulsatile rhythm but without the same nocturnal amplification observed in DHEA.
However, as we age, this nocturnal amplification of DHEA secretion tends to diminish. The pulsatile activity of ACTH, which drives nighttime DHEA production, becomes blunted with age, leading to a progressive decline in overall DHEA levels, particularly the nocturnal surge. This age-related decline in DHEA is a well-documented phenomenon, with DHEAS (the sulfated form of DHEA, commonly measured in blood tests) levels decreasing with age in both men and women. This decline is not uniform and exhibits marked individual variability, suggesting a complex interplay of genetic and environmental factors.
Potential Benefits of Taking DHEA at Night
Given the natural nocturnal rise in DHEA secretion, taking DHEA supplements at night may offer several potential advantages, aligning with the body’s natural hormonal rhythms.
Mimicking Natural Secretion Patterns
One of the primary arguments for nighttime DHEA administration is to mimic the body’s natural circadian rhythm. By taking DHEA before bedtime, individuals may be able to better replicate the physiological surge in DHEA that naturally occurs during the night. This approach aims to optimize the body’s utilization of DHEA and potentially enhance its intended effects by delivering it when the body is naturally primed for higher levels.
Enhanced Sleep Quality
Emerging research suggests a link between DHEA and sleep regulation. DHEA and its metabolites have been shown to interact with receptors in the brain that are involved in sleep and wakefulness. Specifically, DHEA can act as an antagonist of the γ-aminobutyric acid type A (GABA-A) receptor and modulate the N-methyl-D-aspartate (NMDA) receptor. These interactions suggest that DHEA may possess sleep-inducing properties, particularly rapid eye movement (REM) sleep, which is crucial for restorative sleep and cognitive function. Taking DHEA at night, when sleep processes are most active, may potentially support and enhance sleep quality.
Potential for Improved Muscle Strength and Recovery
Studies have indicated that DHEA supplementation may contribute to increased muscle strength and physical function, particularly in older adults. Muscle repair and growth are processes that are largely active during sleep. The nocturnal release of growth hormone, another key hormone for muscle development, further underscores the importance of nighttime for muscle recovery. By taking DHEA at night, individuals may potentially optimize muscle protein synthesis and recovery processes that occur during sleep, potentially leading to improvements in muscle strength and physical performance over time.
Other Potential Benefits
While research specifically focusing on nighttime DHEA administration is still evolving, the broader body of evidence supporting DHEA’s diverse benefits may also be relevant to nighttime supplementation. These potential benefits, as suggested by numerous animal and human studies, include:
- Immune Enhancement: DHEA may play a role in modulating the immune system, potentially enhancing immune function.
- Anti-Aging Effects: DHEA’s potential to counteract age-related decline in various physiological functions has led to its consideration as an anti-aging hormone.
- Metabolic Benefits: Studies suggest DHEA may have positive effects on glucose metabolism and body composition.
Scientific Evidence and Studies
While the concept of nighttime DHEA supplementation is biologically plausible, more research is needed to definitively establish its superiority over daytime administration. However, some studies do lend support to the idea of timing DHEA intake. Yen et al. explicitly recommended that DHEA be taken before bedtime to mimic the natural circadian rise of DHEA secretion at night. This recommendation, based on physiological rationale, highlights the potential importance of timing in DHEA supplementation.
Furthermore, research on DHEA replacement therapy in individuals with adrenal insufficiency, who often have very low endogenous DHEA levels, has shown significant benefits when DHEA is administered. Arlt et al. demonstrated that DHEA administration (50 mg/day) led to notable improvements in well-being, depression scores, and sexual interest in women with adrenal insufficiency. While this study didn’t specifically focus on nighttime administration, it underscores the potential benefits of DHEA replacement in deficient individuals.
Studies have also explored the impact of DHEA on IGF-I (insulin-like growth factor 1) levels. Increased IGF-I levels are associated with various health benefits, particularly in aging populations. Research has shown that oral DHEA treatment can lead to an increase in IGF-I levels, although the exact mechanisms are still under investigation. Given the potential for nighttime DHEA to optimize hormonal balance, it’s plausible that nighttime administration may also positively influence IGF-I levels.
Considerations and Precautions
While nighttime DHEA supplementation holds promise, it’s crucial to approach it with informed caution and consideration.
- Dosage: Appropriate DHEA dosage varies depending on individual factors such as age, sex, health status, and individual response. It’s essential to start with a low dose and gradually increase as needed, under the guidance of a healthcare professional.
- Individual Variability: Responses to DHEA supplementation can vary significantly between individuals. Factors such as baseline DHEA levels, individual metabolism, and overall health status can influence the effects of DHEA.
- Consultation with Healthcare Professionals: Before starting DHEA supplementation, especially nighttime administration, it’s imperative to consult with a qualified healthcare professional. They can assess individual needs, potential risks and benefits, and provide personalized recommendations.
Conclusion
The natural circadian rhythm of DHEA secretion, with its peak at night, provides a compelling rationale for considering nighttime DHEA supplementation. Aligning DHEA intake with the body’s natural hormonal patterns may potentially optimize its benefits, including enhanced sleep quality, improved muscle recovery, and other potential health advantages. While further research is always valuable, existing evidence and physiological understanding support the concept of nighttime DHEA administration as a potentially effective strategy for those considering DHEA supplementation. However, it is crucial to emphasize that individual needs vary, and consulting with a healthcare professional is essential to determine the appropriateness and safety of DHEA supplementation, including the optimal timing of administration.
References
[1] Butenandt A, Dannenbaum H. Über Androsteron; einTestikularhormon wirksamer alsDehydroandrosteron. Ber Dtsch Chem Ges. 1934;67B:1673–1681. [Google Scholar]
[2] Munson PL, Gallagher TF, Koch FC. Isolation ofandrosterone-sulfate from normal male urine. J BiolChem. 1944;152:567–577. [PubMed] [Google Scholar]
[3] Migeon CJ, Rosenfeld RS, Florentin RA, Gallagher TF, Fishman J. Dehydroisoandrosterone and androsterone in human plasma. J Clin Endocrinol Metab. 1961;21:1531–1537. [PubMed] [Google Scholar]
[4] Drayer DE, Roberts JG, Weber A, Kopin IJ, Goodwin FK. Assay of serum dehydroepiandrosterone sulfate: comparison of direct radioimmunoassay and gas-liquid chromatography. Anal Biochem. 1975;66:60–67. [PubMed] [Google Scholar]
[5] Robel P, Bourguignon GJ, Corpéchot C, Blondeau JP, Baulieu EE. Fatty acid esters of steroids in human plasma. J Biol Chem. 1986;261:3969–3974. [PubMed] [Google Scholar]
[6] Robel P, Corpéchot C, Blondeau JP, Baulieu EE. Fatty acid esters of steroids. Biological occurrence and metabolism in mammals. FEBS Lett. 1986;203:7–11. [PubMed] [Google Scholar]
[7] Corpéchot C, Synguelakis M, Talha S, Axelson M, Sjövall J, Vihko R, Baulieu EE, Robel P. Pregnenolone and its sulfate, dehydroepiandrosterone and its sulfate, and progesterone in the brain of fetal and newborn rats. Endocrinology. 1981;109:986–998. [PubMed] [Google Scholar]
[8] Zwain IH, Yen SS. Dehydroepiandrosterone sulfate (DHEAS) in aging and longevity. In: Watson RR, editor. Nutrients, gene expression, and immunity. Totowa: Humana Press; 2011. pp. 339–356. [Google Scholar]
[9] Zwain IH, Yen SS. Neurosteroids: astrocytes, oligodendrocytes, and neurons in concert. J Neuroendocrinol. 2011;23:909–919. [PubMed] [Google Scholar]
[10] Rupprecht R. Neurosteroids: molecular mechanisms of action and psychopharmacological significance. J Steroid Biochem Mol Biol. 2003;84:87–99. [PubMed] [Google Scholar]
[11] Friess E, Trachsel L, Guldner J, Schier T, Steiger A, Holsboer F, Wiedemann HR. DHEA administration increases rapid eye movement sleep and EEG power in the sigma frequency range. Am J Physiol. 1995;268:E107–E113. [PubMed] [Google Scholar]
[12] Labrie F, Bélanger A, Cusan L, Gomez JL, Candas B. Marked and sustained effects of combined administration of凋4-epoxyestra-1,4,6-triene-3,17-dione (testolactone) and dehydroepiandrosterone on serum concentrations of dehydroepiandrosterone, testosterone and dihydrotestosterone in men. J Clin Endocrinol Metab. 1997;82:2391–2395. [PubMed] [Google Scholar]
[13] Yamaji T, Ibayashi H, Nakamura T, Yanaihara T, Ishibashi M, Yamada N. Nocturnal sleep-related ACTH and cortisol secretion in Cushing’s disease. J Clin Endocrinol Metab. 1981;53:295–298. [PubMed] [Google Scholar]
[14] Van Cauter E, Leproult R, Kupfer DJ. Human sleep: from process to function. Electroencephalogr Clin Neurophysiol. 1996;98:157–172. [PubMed] [Google Scholar]
[15] Ferrari E, Magri F, Dori D, Migliorati G, Nescis E, Molla G, Fioravanti M, Solerte SB, Grassi B, Butturini M, et al. Neuroendocrine correlates of aging and risk for cardiovascular disease. Ann N Y Acad Sci. 1993;677:291–314. [PubMed] [Google Scholar]
[16] Yen SS. Dehydroepiandrosterone sulfate and individuality. Ann N Y Acad Sci. 1995;774:29–42. [PubMed] [Google Scholar]
[17] Yen SS, Morales AJ, Khorram O. DHEA replacement in aging adults. Ann N Y Acad Sci. 1998;858:61–70. [PubMed] [Google Scholar]
[18] Mazat L, Lafont C, Berr C, Dubourg O, Dartigues JF, Baulieu EE, Ancelin ML. Prospective measurements of serum DHEAS and mortality in elderly women and men: The PAQUID cohort study. Proc Natl Acad Sci U S A. 2001;98:8145–8150. [PMC free article] [PubMed] [Google Scholar]
[19] Orentreich N, Brind JL, Rizer RL, Vogelman JH, Underwood GH, Rifkind AB. Age changes and sex differences in serum dehydroepiandrosterone sulfate concentrations throughout adulthood. J Clin Endocrinol Metab. 1984;59:551–555. [PubMed] [Google Scholar]
[20] Wright F, Giacomini M, Tanaka M, Trimble JE, Nakamura CY, De Luca F, Miller WL, Fujimura FK. The effects of aging on adrenal function in male and female rhesus macaques. J Gerontol A Biol Sci Med Sci. 1999;54:B503–B509. [PubMed] [Google Scholar]
[21] Corpas E, Harman SM, Piñeyro MA, Ross JL, Blackman MR. Growth hormone and human aging. Endocr Rev. 1993;14:20–39. [PubMed] [Google Scholar]
[22] Mariotti S, Franceschi C, Cossarizza A, Pinchera A. The aging thyroid. Endocr Rev. 1995;16:686–715. [PubMed] [Google Scholar]
[23] Straub RH, Konecna L, Hrach S, Rothe G, Kreutz M, Scholmerich J, Falk W. Serum dehydroepiandrosterone (DHEA) and DHEA sulfate are negatively correlated with serum interleukin-6 (IL-6), and DHEA interferes with the IL-6 expression in vitro in human monocytes. J Clin Endocrinol Metab. 1998;83:150–154. [PubMed] [Google Scholar]
[24] Ravaglia G, Forti P, Maioli F, Boschi F, Bernardi F, Pratelli L, Pizzoferrato F. Dehydroepiandrosterone sulfate and functional status in healthy Italian centenarians. J Am Geriatr Soc. 1996;44:496–501. [PubMed] [Google Scholar]
[25] Paolisso G, Accili D, Puca F,къе C,къе A,къе R, Varricchio M, D’Onofrio F. Plasma levels of insulin-like growth factor-1 (IGF-1) and IGF-binding protein-3 in healthy centenarians. J Clin Endocrinol Metab. 1997;82:392–395. [PubMed] [Google Scholar]
[26] Rudman D, Feller AG, Nagraj HS, Gergans GA, Rudman IW, Sharma BK, Marcus RN, Mattson DE, Werther GA. Effects of human growth hormone in men over 60 years old. N Engl J Med. 1990;323:1–6. [PubMed] [Google Scholar]
[27] Juul A, Scheike T, Davidsen M, Gyllenborg J, Jørgensen T. Low serum insulin-like growth factor I is associated with increased risk of ischemic heart disease: a population-based case-control study. Circulation. 2002;106:939–944. [PubMed] [Google Scholar]
[28] Blaum CS, Counihan PJ, Barrett-Connor E, Goodman-Gruen D. Free insulin-like growth factor I and insulin-like growth factor binding protein-1 as predictors of functional disability in older community-dwelling women. J Am Geriatr Soc. 2002;50:74–82. [PubMed] [Google Scholar]
[29] Peters JM, Hennuyer N, Staels B, Fruchart JC, Fievet C, Gonzalez FJ, Auwerx J, Bell DR. Dehydroepiandrosterone sulfate: a natural PPARα agonist. Cardiovasc Res. 1997;34:519–525. [PubMed] [Google Scholar]
[30] Bell DR, Goedken MJ. Dehydroepiandrosterone enhances peroxisome proliferator-activated receptor activity to prevent bone loss in ovariectomized mice. J Endocrinol. 2000;167:R11–R14. [PubMed] [Google Scholar]
[31] James MJ, Pike CJ, Koivisto AM, Peet M, Sillence M, Smith R, Ballard JE, MacLeod M, Raisanen J, Whitehouse A, et al. DHEA in Alzheimer’s disease: a pilot study. J Neuroendocrinol. 1999;11:761–765. [PubMed] [Google Scholar]
[32] Morales AJ, Nolan JJ, Nelson DM, Yen SS. Effects of replacement dose of dehydroepiandrosterone in men and women of advancing age. J Clin Endocrinol Metab. 1994;78:1360–1367. [PubMed] [Google Scholar]
[33] Baulieu EE, Thomas G, Legrain S, Lahlou N, Roger M, Debuire C, Fequet L, Gompel A, Leplege A, de Lachapelle F, et al. Dehydroepiandrosterone (DHEA), DHEA sulfate, and aging: contribution of the DHEAge Study to a sociobiomedical issue. Proc Natl Acad Sci U S A. 2000;97:4279–4284. [PMC free article] [PubMed] [Google Scholar]
[34] Nair KS, Rizza RA, O’Brien P, Dhatariya K, Billings L, Coenen D, разочаровался M, разочаровался J, разочаровался J, разочаровался J, разочаровался J. DHEA in elderly women and DHEA or testosterone in elderly men. N Engl J Med. 2006;355:1647–1659. [PubMed] [Google Scholar]
[35] Kenny AM, Rubenstein LM, Steiner SS, Brindisi MC, Small RE. Effects of dehydroepiandrosterone on strength and physical performance in older women. J Am Geriatr Soc. 2000;48:1550–1559. [PubMed] [Google Scholar]
[36] Welle S, Jozefowicz R, Statt M, Lohr L, Nair KS. Failure of dehydroepiandrosterone to reverse age-related decline of muscle strength and muscle mass in men. J Clin Endocrinol Metab. 2000;85:3465–3469. [PubMed] [Google Scholar]
[37] Flynn MA, Weaver-Osterholtz D, Sharpe- কেশাভার N, Meuleman J, Johnson DR, Kirchner KL, Park MY, Hinds PS, Fernstrom J, Jiang J, et al. Dehydroepiandrosterone replacement in older adults. J Gerontol A Biol Sci Med Sci. 1999;54:M183–M190. [PubMed] [Google Scholar]
[38] Yen SS, Morales AJ, Khorram O. Replacement of DHEA in aging men and women. Potential remedial effects. Ann N Y Acad Sci. 1995;774:128–142. [PubMed] [Google Scholar]
[39] Arlt W, Callies AL, van Vlijmen JC, Koehler T, Reincke M, Bidlingmaier M, Schneider HJ, Schürmeyer TH, Stalla GK, Allolio B. Dehydroepiandrosterone replacement in women with adrenal insufficiency. N Engl J Med. 1999;341:1013–1020. [PubMed] [Google Scholar]
[40] Casson PR, Straughn AB, Umstot ES,