Why does my vulva hurt? If you’re asking this question, you’re not alone. Vulvar pain is a common issue with many potential causes, ranging from simple irritation to underlying medical conditions. At WHY.EDU.VN, we understand the importance of accurate information and accessible solutions. This comprehensive guide explores the various reasons behind vulvar discomfort, offering insights into diagnosis, treatment, and self-care strategies for your vaginal discomfort and pelvic pain. We also cover related aspects like vaginal burning, vulvar itching, and remedies for vulvar pain.
1. Understanding Vulvar Pain: A Comprehensive Guide
Vulvar pain, also known as vulvodynia, can be a distressing and debilitating condition affecting women of all ages. This guide aims to provide a thorough understanding of the potential causes of vulvar pain, effective strategies for relief, and guidance on when to seek professional medical advice. We delve into the various factors that can contribute to vulvar discomfort, including infections, skin conditions, nerve issues, and lifestyle factors, offering practical tips and solutions to alleviate your symptoms.
2. Common Causes of Vulvar Pain
Several factors can contribute to pain in the vulvar region. Identifying the root cause is crucial for effective treatment. Here are some of the most common culprits:
2.1. Vulvar Irritation
The vulva’s skin is exceptionally sensitive, making it prone to irritation. This irritation can stem from various everyday factors.
-
Irritants: Soaps, detergents, lotions, and douches often contain harsh chemicals that disrupt the natural pH balance of the vulva, leading to dryness, itching, and burning sensations.
-
Clothing: Tight-fitting clothes, especially those made from synthetic materials, can trap moisture and heat, creating an environment conducive to bacterial growth and irritation.
-
Activities: Prolonged sitting, cycling, or horseback riding can cause friction and pressure on the vulva, leading to inflammation and discomfort.
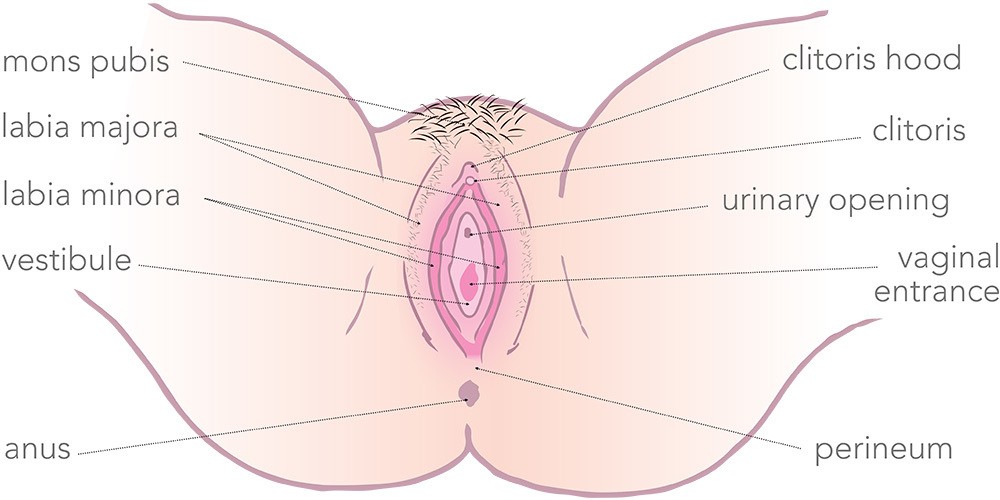 Diagram of the Vulva
Diagram of the Vulva
2.2. Infections
Infections are a frequent cause of vulvar pain, often accompanied by other symptoms like discharge and odor.
- Yeast Infections: Candida overgrowth leads to intense itching, burning, and a thick, white discharge resembling cottage cheese.
- Bacterial Vaginosis (BV): An imbalance of bacteria in the vagina causes a fishy odor, watery discharge, and sometimes vulvar pain.
- Sexually Transmitted Infections (STIs): STIs like herpes, chlamydia, and gonorrhea can manifest as sores, blisters, or inflammation in the vulvar area, leading to significant pain.
2.3. Skin Conditions
Certain skin conditions can specifically target the vulva, causing chronic pain and discomfort.
- Lichen Sclerosus: This chronic inflammatory condition causes white, thin patches of skin on the vulva. It can lead to itching, pain, and even scarring if left untreated.
- Eczema: Also known as atopic dermatitis, eczema can cause dry, itchy, and inflamed skin on the vulva.
- Psoriasis: This autoimmune condition can cause thick, red, scaly patches of skin on the vulva, leading to discomfort and pain.
2.4. Vulvodynia
Vulvodynia is chronic vulvar pain without an identifiable cause. It can be localized (vestibulodynia) or widespread.
- Provoked Vulvodynia: Pain triggered by touch or pressure, such as during sexual activity or tampon insertion.
- Unprovoked Vulvodynia: Constant pain, even without any apparent trigger.
2.5. Nerve-Related Pain
Nerve damage or irritation can also cause vulvar pain.
- Pudendal Neuralgia: Damage to the pudendal nerve, which runs through the pelvis, can cause chronic pain in the vulva, perineum, and rectum.
- Nerve Entrapment: Nerves in the pelvic region can become compressed or trapped, leading to pain and discomfort.
3. Symptoms Associated With Vulvar Pain
Vulvar pain can manifest in various ways, and recognizing these symptoms is crucial for seeking appropriate medical attention.
- Burning: A persistent burning sensation in the vulva.
- Itching: Intense itching that can be difficult to relieve.
- Stinging: A sharp, stinging pain, especially during urination or sexual activity.
- Throbbing: A pulsating or throbbing sensation in the vulvar area.
- Rawness: A feeling of rawness or sensitivity to touch.
- Aching: A dull, constant ache in the vulva.
- Painful Intercourse (Dyspareunia): Pain during or after sexual activity.
- Painful Tampon Insertion: Difficulty or pain when inserting tampons.
- Sensitivity to Touch: Increased sensitivity to touch, making everyday activities like wearing underwear uncomfortable.
- Swelling: Noticeable swelling around the vulva
4. Diagnosing the Cause of Vulvar Pain
Accurately diagnosing the cause of vulvar pain requires a thorough medical evaluation.
4.1. Medical History and Physical Exam
Your doctor will begin by taking a detailed medical history, asking about your symptoms, sexual activity, hygiene practices, and any underlying medical conditions. A physical exam of the vulva and vagina will help identify any visible abnormalities, such as redness, swelling, or lesions.
4.2. Diagnostic Tests
Several diagnostic tests can help determine the cause of vulvar pain.
- Pelvic Exam: A comprehensive examination of the internal and external reproductive organs to identify any abnormalities.
- Cotton Swab Test: A test where a cotton swab is gently touched to different areas of the vulva to identify specific pain points.
- Microscopic Examination of Vaginal Discharge: Helps identify infections like yeast infections or bacterial vaginosis.
- STI Testing: Screening for sexually transmitted infections.
- Biopsy: If a skin condition is suspected, a small tissue sample may be taken for further examination.
5. Treatment Options for Vulvar Pain
Treatment for vulvar pain varies depending on the underlying cause. A combination of medical treatments, self-care strategies, and lifestyle modifications can provide relief.
5.1. Medical Treatments
- Topical Medications: Creams and ointments containing corticosteroids, anesthetics, or antifungal agents can help reduce inflammation, pain, and itching.
- Oral Medications: Pain relievers, antidepressants, and nerve pain medications can help manage chronic vulvar pain.
- Nerve Blocks: Injections of local anesthetics can block pain signals from the nerves in the vulvar area.
- Physical Therapy: Pelvic floor physical therapy can help strengthen and relax the pelvic floor muscles, reducing pain and improving sexual function.
- Surgery: In rare cases, surgery may be necessary to remove painful tissue or correct structural abnormalities.
5.2. Self-Care Strategies
- Gentle Cleansing: Wash the vulva with warm water only, avoiding harsh soaps and detergents.
- Loose Clothing: Wear loose-fitting, cotton underwear to allow the skin to breathe and reduce irritation.
- Avoid Irritants: Avoid using douches, feminine hygiene sprays, and scented products.
- Cool Compresses: Apply cool compresses to the vulva to relieve pain and itching.
- Sitz Baths: Soak in a warm sitz bath for 10-15 minutes several times a day to soothe irritated tissues.
5.3. Lifestyle Modifications
- Diet: A balanced diet rich in fruits, vegetables, and whole grains can support overall health and reduce inflammation.
- Exercise: Regular exercise can improve circulation and reduce stress, both of which can help manage vulvar pain.
- Stress Management: Practice relaxation techniques like yoga, meditation, or deep breathing to reduce stress and anxiety, which can exacerbate vulvar pain.
6. When to Seek Professional Help
While many cases of vulvar pain can be managed with self-care strategies, it is essential to seek professional medical advice in certain situations.
- Severe Pain: If the pain is severe and interferes with daily activities.
- Persistent Pain: If the pain lasts for more than a few weeks despite self-care measures.
- Unexplained Symptoms: If you experience other symptoms like fever, chills, or unexplained weight loss.
- Changes in Skin: If you notice any changes in the skin of the vulva, such as sores, blisters, or thickening.
- Painful Intercourse: If you experience persistent pain during or after sexual activity.
7. Vulvar Pain and Sexual Health
Vulvar pain can significantly impact sexual health and intimacy. It can lead to painful intercourse, decreased libido, and difficulty achieving orgasm.
7.1. Communicating With Your Partner
Open communication with your partner is essential. Explain your condition and how it affects you. Work together to find ways to maintain intimacy and connection.
7.2. Experimenting With Different Positions
Experiment with different sexual positions to find ones that are more comfortable. Positions that minimize pressure on the vulva may be helpful.
7.3. Using Lubricants
Use a generous amount of water-based lubricant during sexual activity to reduce friction and pain.
7.4. Seeking Professional Counseling
A sex therapist or counselor can provide guidance and support in addressing the emotional and relational challenges associated with vulvar pain.
8. The Role of Pelvic Floor Physical Therapy
Pelvic floor physical therapy can be an effective treatment for vulvar pain, particularly in cases of vulvodynia and nerve-related pain.
8.1. Strengthening Weak Muscles
Weak pelvic floor muscles can contribute to vulvar pain. Physical therapy exercises can help strengthen these muscles, providing support and stability.
8.2. Releasing Tight Muscles
Tight pelvic floor muscles can also cause pain and discomfort. Physical therapy techniques like massage and stretching can help release tension and improve blood flow.
8.3. Improving Nerve Function
Physical therapy can help improve nerve function in the pelvic region, reducing pain and sensitivity.
9. Understanding Vulvodynia in Detail
Vulvodynia, characterized by chronic pain in the vulva without an identifiable cause, presents unique challenges.
9.1. Types of Vulvodynia
- Localized Vulvodynia: Pain is confined to a specific area of the vulva, such as the vestibule (the area around the vaginal opening).
- Generalized Vulvodynia: Pain is more widespread, affecting the entire vulva.
9.2. Factors Contributing to Vulvodynia
- Nerve Damage or Irritation: Damage to the nerves in the vulva can cause chronic pain.
- Genetic Factors: Some women may be genetically predisposed to developing vulvodynia.
- Hormonal Factors: Hormonal imbalances may play a role in vulvodynia.
- Pelvic Floor Dysfunction: Tight or weak pelvic floor muscles can contribute to vulvodynia.
- Inflammatory Conditions: Chronic inflammation in the vulvar area may lead to vulvodynia.
9.3. Treatment Approaches for Vulvodynia
- Medications: Topical creams, oral pain relievers, and nerve pain medications can help manage vulvodynia symptoms.
- Physical Therapy: Pelvic floor physical therapy can help improve muscle function and reduce pain.
- Cognitive Behavioral Therapy (CBT): CBT can help women cope with chronic pain and improve their quality of life.
- Surgery: In some cases, surgery may be an option to remove painful tissue.
10. Lichen Sclerosus: A Closer Look
Lichen sclerosus is a chronic skin condition that primarily affects the vulva and anus.
10.1. Symptoms of Lichen Sclerosus
- White Patches: White, thin patches of skin on the vulva.
- Itching: Intense itching that can be difficult to relieve.
- Pain: Pain and discomfort in the vulvar area.
- Thinning Skin: Thinning of the skin, making it more prone to tearing.
- Scarring: Scarring and changes in the shape of the vulva.
10.2. Diagnosing Lichen Sclerosus
Lichen sclerosus is typically diagnosed based on a physical exam and a biopsy of the affected skin.
10.3. Treatment for Lichen Sclerosus
- Topical Corticosteroids: These medications can help reduce inflammation and itching.
- Regular Monitoring: Women with lichen sclerosus need regular monitoring due to a slightly increased risk of vulvar cancer.
11. Vulvar Pain After Childbirth
Childbirth can cause trauma to the vulva and perineum, leading to pain and discomfort.
11.1. Vaginal Tears
Vaginal tears are common during childbirth and can range from minor to severe.
11.2. Episiotomy
An episiotomy is a surgical incision made to enlarge the vaginal opening during childbirth.
11.3. Recovery From Childbirth
- Pain Management: Pain relievers can help manage pain and discomfort.
- Sitz Baths: Warm sitz baths can soothe irritated tissues.
- Perineal Care: Keeping the perineal area clean and dry is essential for healing.
- Pelvic Floor Exercises: Pelvic floor exercises can help strengthen the pelvic floor muscles and improve recovery.
12. Preventing Vulvar Pain
Taking preventive measures can help reduce the risk of developing vulvar pain.
12.1. Good Hygiene Practices
- Gentle Cleansing: Wash the vulva with warm water only.
- Avoid Irritants: Avoid using harsh soaps, douches, and scented products.
- Proper Wiping Technique: Wipe from front to back after using the toilet.
12.2. Healthy Lifestyle
- Balanced Diet: Eat a balanced diet rich in fruits, vegetables, and whole grains.
- Regular Exercise: Engage in regular exercise to improve circulation and reduce stress.
- Stress Management: Practice relaxation techniques to manage stress.
12.3. Safe Sex Practices
- Use Condoms: Use condoms during sexual activity to prevent STIs.
- Regular STI Testing: Get regular STI testing, especially if you have multiple partners.
13. Exploring Natural Remedies for Vulvar Pain
While medical treatments are often necessary, some natural remedies can provide relief from vulvar pain.
13.1. Herbal Remedies
- Calendula: Calendula cream can help soothe irritated skin.
- Chamomile: Chamomile tea or compresses can help reduce inflammation.
- Tea Tree Oil: Diluted tea tree oil can help fight infections.
13.2. Homeopathic Remedies
- Arnica: Arnica can help reduce pain and swelling.
- Hypericum: Hypericum can help relieve nerve pain.
13.3. Other Natural Remedies
- Coconut Oil: Coconut oil can help moisturize and soothe dry skin.
- Aloe Vera: Aloe vera gel can help heal irritated skin.
- Vitamin E Oil: Vitamin E oil can help nourish and protect the skin.
Disclaimer: Always consult with your healthcare provider before using any natural remedies, especially if you are pregnant, breastfeeding, or have any underlying medical conditions.
14. Frequently Asked Questions (FAQs) About Vulvar Pain
Here are some frequently asked questions about vulvar pain:
- What is vulvodynia? Vulvodynia is chronic vulvar pain without an identifiable cause.
- What are the symptoms of lichen sclerosus? Symptoms include white patches, itching, pain, thinning skin, and scarring.
- Can vulvar pain affect my sex life? Yes, vulvar pain can lead to painful intercourse, decreased libido, and difficulty achieving orgasm.
- What are some self-care strategies for vulvar pain? Gentle cleansing, loose clothing, avoiding irritants, and cool compresses can provide relief.
- When should I see a doctor for vulvar pain? See a doctor if the pain is severe, persistent, or accompanied by other symptoms like fever or changes in the skin.
- What is pelvic floor physical therapy? Pelvic floor physical therapy helps strengthen and relax the pelvic floor muscles, reducing pain and improving sexual function.
- Can stress cause vulvar pain? Yes, stress can exacerbate vulvar pain.
- Are there any natural remedies for vulvar pain? Herbal remedies like calendula and chamomile can provide relief.
- Can childbirth cause vulvar pain? Yes, vaginal tears and episiotomies during childbirth can cause vulvar pain.
- How can I prevent vulvar pain? Good hygiene practices, a healthy lifestyle, and safe sex practices can help reduce the risk.
15. Latest Research and Updates on Vulvar Pain
Stay informed about the latest advancements in vulvar pain research and treatment options.
| Research Area | Key Findings | Implications for Treatment |
|---|---|---|
| Neuropathic Pain Mechanisms | Identified specific nerve pathways involved in vulvodynia pain. | Development of targeted therapies |
| Genetic Predisposition | Discovered genetic markers associated with increased risk of vulvodynia. | Personalized prevention strategies |
| Pelvic Floor Muscle Dysfunction | Confirmed the role of pelvic floor muscle tension in contributing to vulvar pain. | Enhanced physical therapy techniques |
| Psychological Factors | Highlighted the impact of anxiety and depression on the perception of vulvar pain. | Integrated mental health support |
| Novel Topical Treatments | Evaluated the effectiveness of new topical creams and ointments for pain relief. | Improved symptom management |
16. Connecting with the WHY.EDU.VN Community
At WHY.EDU.VN, we understand the challenges of finding accurate and trustworthy information. Our website is designed to provide comprehensive answers and connect you with experts who can address your specific concerns.
- Ask Questions: Our platform allows you to ask questions and receive answers from knowledgeable professionals.
- Explore Topics: Dive into a wide range of subjects, from science and history to health and technology.
- Join the Community: Engage with other users, share your experiences, and learn from diverse perspectives.
If you’re seeking reliable answers and a supportive community, look no further than WHY.EDU.VN.
Address: 101 Curiosity Lane, Answer Town, CA 90210, United States
WhatsApp: +1 (213) 555-0101
Website: WHY.EDU.VN
Conclusion
Dealing with vulvar pain can be challenging, but understanding the potential causes and available treatment options is the first step toward finding relief. Remember, you are not alone, and help is available. At WHY.EDU.VN, we are committed to providing you with accurate information, expert advice, and a supportive community to guide you on your journey to better health. Don’t hesitate to reach out and ask questions – our team of experts is here to help.
If you’re struggling to find the answers you need or feel overwhelmed by the complexities of vulvar pain, we encourage you to visit WHY.EDU.VN today. Our platform connects you with specialists who can provide personalized guidance and support, ensuring you receive the most effective care possible. Take the first step towards relief and a better quality of life – your questions deserve expert answers, and you’ll find them at why.edu.vn.