While discussing bowel movements might feel awkward, it’s a universal aspect of health. In fact, the characteristics of your poop, including its color, can offer valuable insights into your digestive well-being. Experts in digestive health emphasize that observing your stool is a simple yet effective way to monitor your gut health. Let’s delve into the common question: Why Is Poop Brown and what other colors might indicate about your health.
The Science Behind Brown Poop: Bilirubin and Digestion
Poop’s typical brown color is a result of a fascinating process linked to your liver and digestion. This signature hue comes from a pigment called bilirubin, which is created during the breakdown of hemoglobin. Hemoglobin is a protein found in red blood cells. Here’s a step-by-step breakdown of how poop gets its brown color:
- Hemoglobin Breakdown: When red blood cells reach the end of their lifespan, they are broken down in the liver. During this process, hemoglobin is converted into bilirubin.
- Bilirubin and Bile: The liver then releases bilirubin into bile, a fluid that aids in the digestion of fats in the small intestine. Bile is initially greenish-yellow in color due to bilirubin.
- Journey Through the Intestines: Bile, containing bilirubin, travels from the liver to the gallbladder (where it’s stored) and then into the small intestine. As bile moves through the digestive tract, it undergoes further chemical changes by enzymes.
- Bacterial Action in the Large Intestine: Once bilirubin reaches the large intestine (colon), it interacts with bacteria. These bacteria further modify bilirubin into compounds called urobilinogens, and then further into stercobilin.
- Stercobilin: The Brown Pigment: Stercobilin is the pigment that gives poop its characteristic brown color. The longer stool stays in the large intestine, the more time bacteria have to work on bilirubin, typically resulting in that familiar brown shade.
Essentially, poop is brown because of stercobilin, a byproduct of bilirubin breakdown by bacteria in your gut. If your digestive system is functioning correctly, allowing stool to move through at a normal pace, there’s sufficient time for this process to complete, resulting in healthy brown poop, often likened to the color of a milk chocolate bar.
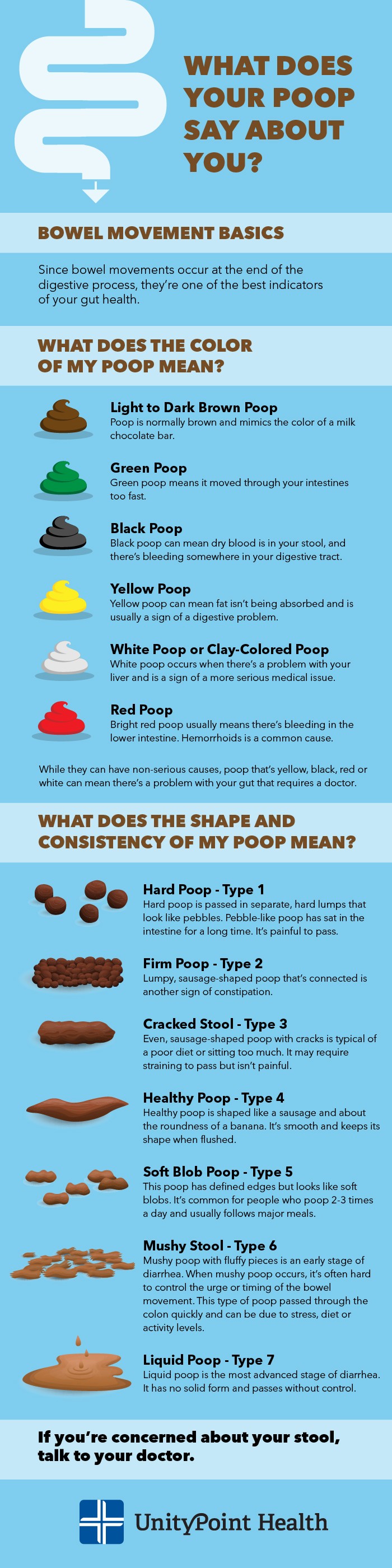
What Different Poop Colors Mean? Beyond Brown
While brown is the norm, poop can come in a rainbow of colors, each potentially signaling different things about your health. Here’s a guide to understanding what various poop colors might indicate:
Green Poop: Diet and Transit Time
Seeing green poop occasionally isn’t usually cause for alarm. As mentioned earlier, bile itself is greenish. If stool moves through the intestines too quickly, bile doesn’t have enough time to undergo the complete color change to brown. This rapid transit can be due to:
- Diet: Consuming large amounts of green leafy vegetables like spinach, kale, or foods with green food coloring can lead to green stool.
- Diarrhea: When you have diarrhea, food passes through your digestive system faster, which can result in green poop.
Other potential causes of green poop:
- Iron supplements: Can sometimes cause green stool.
- Antibiotics: Can alter gut bacteria, potentially leading to color changes.
- Infections: Bacterial or viral infections can speed up digestion.
- Gastrointestinal disorders: Conditions like Crohn’s disease or celiac disease can sometimes result in green stool.
While occasional green poop isn’t usually concerning, persistent green stool, especially if accompanied by other symptoms like diarrhea or abdominal pain, should be discussed with a healthcare provider.
Black Poop: Potential Upper GI Bleeding
Black stool is a more serious color change and warrants prompt medical attention. Black, tarry stool (melena) often indicates the presence of digested blood. This usually points to bleeding in the upper gastrointestinal (GI) tract, such as the esophagus, stomach, or duodenum. The blood becomes darkened and tarry as it travels through the digestive system and is digested.
Seek immediate medical advice if you notice black stool.
Other potential (less serious) causes of black poop:
- Iron supplements: Can sometimes cause dark, almost black stool, but it’s usually not tarry.
- Black foods: Eating large quantities of black licorice, blueberries, or foods with black food coloring can temporarily darken stool.
- Bismuth subsalicylate (Pepto-Bismol): This medication can also cause black stool.
It’s crucial to differentiate between black stool due to medication or diet and black stool due to blood. If you’re unsure, or if you have other symptoms like abdominal pain, dizziness, or weakness, it’s always best to consult a doctor.
Yellow Poop: Fat Malabsorption
Yellow poop, particularly if it’s also greasy and foul-smelling, can indicate fat malabsorption. This means your body isn’t properly absorbing fat from your diet. This can be caused by various conditions affecting the pancreas, liver, gallbladder, or small intestine:
- Pancreatic issues: Conditions like pancreatitis or cystic fibrosis can impair the pancreas’s ability to produce enzymes needed to digest fat.
- Liver and gallbladder problems: Issues affecting bile production or flow can hinder fat digestion.
- Celiac disease: Damage to the small intestine lining in celiac disease can impair nutrient absorption, including fat.
- Infections: Parasitic infections like giardiasis can also lead to fat malabsorption.
If you consistently have yellow, greasy stool, it’s important to consult a doctor to determine the underlying cause.
It’s worth noting that sometimes yellowish-brown or pale stool can be mistaken for yellow poop. Pale stool tends to have a more grayish tint and may be less greasy.
Pale White or Clay-Colored Poop: Bile Duct Obstruction
Pale, white, or clay-colored stool is another color change that can signal a more serious problem. This color often indicates a lack of bile in the stool. Bile is what gives poop its brown color, so if bile production or flow is blocked, stool can become pale. This can be due to:
- Bile duct obstruction: Blockages in the bile ducts, often caused by gallstones or tumors, can prevent bile from reaching the intestines.
- Liver problems: Conditions affecting the liver’s ability to produce or release bile can also lead to pale stool.
Pale stool is often a sign of a potentially serious underlying condition. If you experience pale or clay-colored stool for more than a day or two, seek medical attention.
Red Poop: Lower GI Bleeding or Diet
Red poop is often alarming, but it’s not always a sign of a serious problem. Bright red blood in stool (hematochezia) usually indicates bleeding in the lower GI tract, such as the rectum or anus. Common causes include:
- Hemorrhoids: Swollen veins in the rectum and anus are a frequent cause of bright red blood in stool.
- Anal fissures: Small tears in the lining of the anus can also cause bleeding.
- Inflammatory bowel disease (IBD): Conditions like ulcerative colitis and Crohn’s disease can cause bleeding in the intestines.
- Diverticulitis: Inflammation or infection of small pouches in the colon can lead to bleeding.
- Polyps or colon cancer: While less common, these conditions can also cause rectal bleeding.
Less serious causes of red poop:
- Red food dyes: Consuming foods with red food coloring, like fruit punch, red gelatin, or beets, can temporarily turn stool reddish.
While dietary causes are possible, it’s crucial to rule out bleeding as the cause of red stool. If you see bright red blood in your stool, it’s important to consult your doctor to determine the cause and receive appropriate treatment.
 What is Your Poop Trying to Tell You article
What is Your Poop Trying to Tell You article
What Does the Shape and Consistency of My Stool Say? The Bristol Stool Chart
Beyond color, the shape and consistency of your poop are also important indicators of digestive health. Factors like diet, hydration, medication, and the time poop spends in your intestines influence stool form. The Bristol Stool Chart is a helpful tool for classifying stool types and understanding what they might mean:
- Type 1: Separate Hard Lumps (Pebbles): Indicates severe constipation. Stool has been in the colon for a long time, losing water and becoming hard.
- Type 2: Sausage-Shaped but Lumpy: Also indicates constipation, but less severe than Type 1. Stool has been in the colon for a while and is dehydrated.
- Type 3: Sausage-Shaped with Cracks on the Surface: Represents mild constipation. Often associated with a poor diet or lack of physical activity.
- Type 4: Sausage-Shaped, Smooth and Soft: Considered “normal” and healthy. Easy to pass.
- Type 5: Soft Blobs with Defined Edges: Indicates a lack of fiber. Stool is moving through the colon a bit faster than ideal.
- Type 6: Mushy, Fluffy Pieces with Ragged Edges: Suggests diarrhea. Stool is moving through the colon too quickly, and there’s excess water.
- Type 7: Liquid, No Solid Pieces: Indicates diarrhea. Stool has passed through the colon very rapidly, with minimal water absorption.
Understanding the Bristol Stool Chart can help you track your bowel health and identify potential issues. Aim for Type 3 or Type 4 stool for optimal digestive health.
When to Be Concerned About Your Poop
Observing your poop is a simple way to monitor your digestive health. While occasional variations in color and consistency are normal, certain changes warrant medical attention. Consult your doctor if you experience any of the following:
- Persistent changes in stool color: Especially black, pale, or persistently yellow stool.
- Blood in your stool: Bright red or black, tarry stool.
- Changes in bowel habits: Such as new onset constipation or diarrhea that lasts for more than a few days.
- Abdominal pain, cramping, bloating, or unexplained weight loss along with changes in stool.
Don’t hesitate to discuss your bowel movements with your doctor. It’s a crucial aspect of your overall health, and addressing concerns early can help prevent more serious problems.