Is your poop frequently soft? At WHY.EDU.VN, we understand that changes in stool consistency can be concerning, so let’s delve into the possible causes of soft stool and explore what it might indicate about your digestive health. This comprehensive guide will cover everything from dietary influences to underlying medical conditions, offering practical advice on when to seek medical attention and simple remedies to improve your stool consistency and digestive wellness. Understand loose stools, bowel health, and gastrointestinal function.
1. Understanding Soft Stool: An Overview
Soft stool, often referred to as loose stool, is a common digestive issue characterized by a change in the consistency of bowel movements. Instead of being firm and formed, the stool becomes watery, mushy, or semi-solid. While occasional soft stool is usually not a cause for concern, persistent or frequent occurrences can indicate an underlying digestive problem or dietary imbalance. Understanding the various factors that can influence stool consistency is essential for maintaining good digestive health.
1.1. What Constitutes Soft Stool?
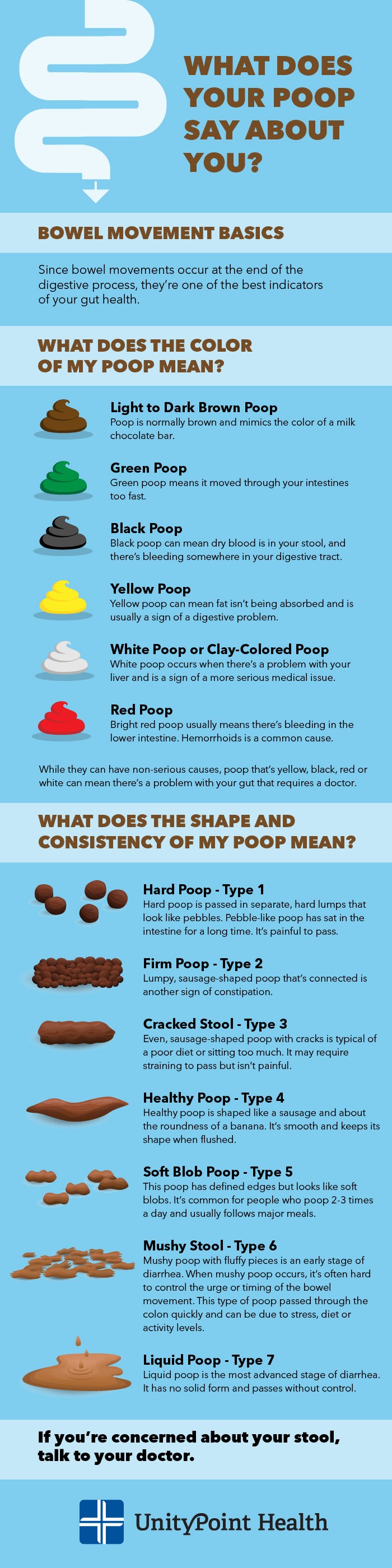
Soft stool is defined as bowel movements that are loose, watery, or unformed. Unlike normal, healthy stool, which is typically solid and easy to pass, soft stool lacks shape and often has a mushy or liquid consistency. The Bristol Stool Chart, a diagnostic tool used to classify the form of human feces into seven categories, can help identify soft stool. Types 5, 6, and 7 on the Bristol Stool Chart indicate varying degrees of soft stool, ranging from soft blobs with defined edges to completely liquid stool.
1.2. The Bristol Stool Chart
The Bristol Stool Chart is a visual aid developed by Dr. Stephen Lewis and Dr. Ken Heaton at the University of Bristol to classify the form of human feces into seven categories. This chart is widely used in clinical settings to help patients describe their bowel movements and assist healthcare professionals in assessing digestive health. The chart categories range from hard, separate lumps (Type 1) to entirely liquid stool (Type 7), providing a standardized way to evaluate stool consistency.
| Type | Description | Characteristics | Implications |
|---|---|---|---|
| 1 | Separate hard lumps, like nuts (hard to pass) | Hard, pebble-like | Severe constipation, lack of fiber |
| 2 | Sausage-shaped, but lumpy | Firm, elongated, lumpy | Constipation, slow transit time |
| 3 | Like a sausage but with cracks on its surface | Formed, cracked surface | Normal, but could indicate mild constipation |
| 4 | Like a sausage or snake, smooth and soft | Smooth, soft, easy to pass | Ideal stool consistency |
| 5 | Soft blobs with clear-cut edges (passed easily) | Soft, separate pieces | Lacking fiber, frequent bowel movements |
| 6 | Fluffy pieces with ragged edges, a mushy stool | Mushy, inconsistent | Mild diarrhea, rapid transit time |
| 7 | Watery, no solid pieces (entirely liquid) | Liquid, no form | Severe diarrhea, infection |
1.3. Frequency of Bowel Movements and Soft Stool
The frequency of bowel movements varies from person to person, but generally, having bowel movements between three times a day and three times a week is considered normal. However, if you experience soft stool more frequently than usual, it may indicate an underlying issue. Pay attention to any changes in your bowel habits, such as increased frequency, urgency, or persistent soft stool, and consult a healthcare professional if these symptoms persist.
1.4. Temporary vs. Chronic Soft Stool
Soft stool can be either temporary or chronic, depending on the underlying cause and duration of symptoms. Temporary soft stool is often caused by dietary changes, stress, or a mild infection and usually resolves within a few days. Chronic soft stool, on the other hand, persists for several weeks or months and may be a sign of a more serious digestive disorder. If you experience chronic soft stool, it’s important to seek medical attention to determine the cause and receive appropriate treatment.
2. Common Causes of Soft Stool
Several factors can contribute to soft stool, ranging from dietary choices and lifestyle habits to underlying medical conditions and medications. Identifying the potential causes of your soft stool can help you take appropriate steps to manage your symptoms and improve your digestive health.
2.1. Dietary Factors
Diet plays a significant role in stool consistency. Certain foods and dietary habits can lead to soft stool, while others can help promote healthy bowel movements.
2.1.1. High-Fiber Intake
While fiber is essential for digestive health, consuming too much fiber, especially suddenly, can lead to soft stool. Fiber absorbs water in the intestines, and excessive intake can result in loose, watery bowel movements. Gradually increase your fiber intake to allow your digestive system to adjust.
2.1.2. Spicy Foods
Spicy foods can stimulate the digestive system and accelerate the passage of stool through the intestines, leading to soft stool. Capsaicin, the active compound in chili peppers, can irritate the intestinal lining and cause diarrhea.
2.1.3. Fatty Foods
High-fat foods can be difficult to digest and may cause soft stool. Fat malabsorption can occur when the body is unable to properly break down and absorb fats, resulting in oily, loose stool.
2.1.4. Artificial Sweeteners
Artificial sweeteners, such as sorbitol, mannitol, and xylitol, are commonly found in sugar-free products. These sweeteners can have a laxative effect and cause soft stool, especially when consumed in large quantities.
2.1.5. Dairy Products (Lactose Intolerance)
Lactose intolerance is a common condition in which the body is unable to digest lactose, a sugar found in dairy products. Consuming dairy products can cause soft stool, bloating, gas, and abdominal pain in individuals with lactose intolerance.
2.1.6. Caffeine and Alcohol
Caffeine and alcohol can stimulate the digestive system and increase bowel motility, leading to soft stool. Both substances can also have a diuretic effect, causing dehydration and further affecting stool consistency.
 Dietary factors impacting stool consistency
Dietary factors impacting stool consistency
2.2. Infections and Illnesses
Infections and illnesses can disrupt the normal function of the digestive system, leading to soft stool and other gastrointestinal symptoms.
2.2.1. Viral Gastroenteritis (Stomach Flu)
Viral gastroenteritis, commonly known as the stomach flu, is an infection of the digestive system caused by viruses such as norovirus and rotavirus. Symptoms include soft stool, nausea, vomiting, abdominal cramps, and fever.
2.2.2. Bacterial Infections (e.g., E. coli, Salmonella)
Bacterial infections, such as those caused by E. coli and Salmonella, can result in food poisoning and lead to soft stool, abdominal pain, fever, and vomiting. These infections are often contracted through contaminated food or water.
2.2.3. Parasitic Infections (e.g., Giardia)
Parasitic infections, such as giardiasis, can cause soft stool, abdominal cramps, bloating, and nausea. Giardia is a parasite that infects the small intestine and is often contracted through contaminated water.
2.2.4. Irritable Bowel Syndrome (IBS)
Irritable Bowel Syndrome (IBS) is a chronic gastrointestinal disorder that affects the large intestine. IBS can cause a variety of symptoms, including soft stool, abdominal pain, bloating, gas, and changes in bowel habits.
2.2.5. Inflammatory Bowel Disease (IBD)
Inflammatory Bowel Disease (IBD) is a group of chronic inflammatory conditions that affect the digestive tract, including Crohn’s disease and ulcerative colitis. IBD can cause soft stool, abdominal pain, rectal bleeding, weight loss, and fatigue.
2.3. Medications and Supplements
Certain medications and supplements can disrupt the normal function of the digestive system, leading to soft stool as a side effect.
2.3.1. Antibiotics
Antibiotics can kill beneficial bacteria in the gut, disrupting the balance of the gut microbiome and leading to soft stool. Antibiotic-associated diarrhea is a common side effect of antibiotic use.
2.3.2. Laxatives
Laxatives are medications used to treat constipation, but overuse can lead to soft stool and diarrhea. Laxatives work by stimulating bowel movements or drawing water into the intestines, which can result in loose, watery stool.
2.3.3. Antacids Containing Magnesium
Antacids containing magnesium can have a laxative effect and cause soft stool. Magnesium can draw water into the intestines, leading to increased bowel motility and loose stool.
2.3.4. Chemotherapy Drugs
Chemotherapy drugs can damage the cells lining the digestive tract, leading to soft stool, nausea, vomiting, and loss of appetite. Chemotherapy-induced diarrhea is a common side effect of cancer treatment.
2.3.5. Iron Supplements
Iron supplements can cause digestive upset, including soft stool, constipation, abdominal pain, and nausea. Iron can irritate the lining of the digestive tract and disrupt normal bowel function.
2.4. Lifestyle Factors
Lifestyle factors, such as stress, anxiety, and changes in routine, can also contribute to soft stool.
2.4.1. Stress and Anxiety
Stress and anxiety can affect the digestive system by increasing gut motility and altering the balance of gut bacteria. Stress-related diarrhea is a common condition in which stress triggers soft stool and abdominal discomfort.
2.4.2. Travel and Changes in Routine
Travel and changes in routine can disrupt the normal function of the digestive system, leading to soft stool. Changes in diet, water, and sleep patterns can all contribute to digestive upset.
3. Symptoms Associated with Soft Stool
Soft stool can be accompanied by a variety of symptoms, depending on the underlying cause. Recognizing these symptoms can help you determine the severity of your condition and seek appropriate medical attention.
3.1. Abdominal Pain and Cramping
Abdominal pain and cramping are common symptoms associated with soft stool. These symptoms can range from mild discomfort to severe pain and may be caused by inflammation, infection, or increased bowel motility.
3.2. Bloating and Gas
Bloating and gas are also common symptoms of soft stool. These symptoms can be caused by excessive gas production in the intestines, which may result from bacterial fermentation of undigested food or impaired nutrient absorption.
3.3. Nausea and Vomiting
Nausea and vomiting can accompany soft stool, particularly in cases of infection or food poisoning. These symptoms may be caused by irritation of the digestive tract or the body’s attempt to eliminate harmful substances.
3.4. Urgency and Frequent Bowel Movements
Urgency and frequent bowel movements are characteristic of soft stool. You may experience a sudden and uncontrollable urge to have a bowel movement, and you may need to go to the bathroom more frequently than usual.
3.5. Dehydration
Dehydration can occur as a result of soft stool, especially if you are experiencing frequent bowel movements. Dehydration can lead to symptoms such as thirst, dizziness, fatigue, and decreased urination.
3.6. Weight Loss
Weight loss can occur in cases of chronic soft stool, particularly if it is caused by malabsorption or inflammatory bowel disease. Impaired nutrient absorption can lead to weight loss and malnutrition.
3.7. Fatigue
Fatigue is a common symptom associated with chronic soft stool. Persistent digestive upset and nutrient malabsorption can lead to fatigue, weakness, and decreased energy levels.
4. Diagnosing the Cause of Soft Stool
Diagnosing the cause of soft stool requires a thorough evaluation of your medical history, symptoms, and lifestyle factors. Your healthcare provider may recommend various diagnostic tests to identify the underlying cause of your symptoms.
4.1. Medical History and Physical Examination
Your healthcare provider will begin by taking a detailed medical history, asking about your symptoms, bowel habits, diet, medications, and any underlying medical conditions. They will also perform a physical examination to assess your overall health and identify any signs of digestive distress.
4.2. Stool Tests
Stool tests can help identify infections, inflammation, and other abnormalities in your digestive system. Common stool tests include:
4.2.1. Stool Culture
A stool culture can identify bacteria, viruses, and parasites that may be causing your soft stool. This test involves collecting a stool sample and sending it to a laboratory for analysis.
4.2.2. Fecal Occult Blood Test (FOBT)
A fecal occult blood test (FOBT) can detect hidden blood in your stool, which may indicate bleeding in the digestive tract. This test is often used to screen for colorectal cancer and other digestive disorders.
4.2.3. Fecal Calprotectin Test
A fecal calprotectin test measures the level of calprotectin, a protein released by white blood cells, in your stool. Elevated levels of calprotectin can indicate inflammation in the digestive tract, which may be a sign of inflammatory bowel disease (IBD).
4.2.4. Stool Fat Test
A stool fat test measures the amount of fat in your stool, which can help diagnose fat malabsorption. This test involves collecting stool samples over a period of several days and sending them to a laboratory for analysis.
4.3. Blood Tests
Blood tests can help assess your overall health and identify any underlying medical conditions that may be contributing to your soft stool. Common blood tests include:
4.3.1. Complete Blood Count (CBC)
A complete blood count (CBC) measures the levels of red blood cells, white blood cells, and platelets in your blood. This test can help detect infections, anemia, and other blood disorders.
4.3.2. Electrolyte Panel
An electrolyte panel measures the levels of electrolytes, such as sodium, potassium, and chloride, in your blood. Electrolyte imbalances can occur as a result of dehydration caused by soft stool.
4.3.3. Liver Function Tests (LFTs)
Liver function tests (LFTs) measure the levels of enzymes and proteins in your blood that are produced by the liver. Abnormal LFT results may indicate liver disease or other liver-related problems.
4.3.4. Thyroid Function Tests
Thyroid function tests measure the levels of thyroid hormones in your blood. Thyroid disorders can affect bowel function and lead to soft stool or constipation.
4.4. Imaging Tests
Imaging tests can help visualize the digestive tract and identify any structural abnormalities that may be causing your soft stool. Common imaging tests include:
4.4.1. Colonoscopy
A colonoscopy involves inserting a long, flexible tube with a camera into your rectum to examine the entire colon. This test can help detect polyps, tumors, inflammation, and other abnormalities in the colon.
4.4.2. Sigmoidoscopy
A sigmoidoscopy is similar to a colonoscopy, but it only examines the lower portion of the colon (sigmoid colon). This test can help detect abnormalities in the rectum and sigmoid colon.
4.4.3. Upper Endoscopy
An upper endoscopy involves inserting a long, flexible tube with a camera into your mouth to examine the esophagus, stomach, and duodenum. This test can help detect ulcers, inflammation, and other abnormalities in the upper digestive tract.
4.4.4. Abdominal X-ray
An abdominal X-ray can help visualize the organs in your abdomen and identify any blockages, perforations, or other abnormalities.
4.5. Food Diary and Elimination Diet
Keeping a food diary and following an elimination diet can help identify food sensitivities or intolerances that may be contributing to your soft stool.
4.5.1. Food Diary
A food diary involves recording everything you eat and drink, along with any symptoms you experience, over a period of several days or weeks. This can help you identify patterns and potential triggers for your soft stool.
4.5.2. Elimination Diet
An elimination diet involves removing certain foods from your diet for a period of several weeks and then gradually reintroducing them to see if they trigger any symptoms. Common foods to eliminate include dairy, gluten, soy, and artificial sweeteners.
5. Treatment Options for Soft Stool
The treatment for soft stool depends on the underlying cause and severity of your symptoms. In many cases, simple lifestyle changes and over-the-counter remedies can help relieve symptoms. However, if your soft stool is caused by an underlying medical condition, you may need more specific treatment.
5.1. Dietary Modifications
Making changes to your diet can often help improve stool consistency and reduce symptoms of soft stool.
5.1.1. BRAT Diet
The BRAT diet (bananas, rice, applesauce, toast) is a bland diet that can help firm up stool and relieve diarrhea. These foods are easy to digest and low in fiber, which can help slow down bowel movements.
5.1.2. Increase Soluble Fiber Intake
Soluble fiber absorbs water in the intestines, which can help firm up stool. Good sources of soluble fiber include oats, barley, apples, citrus fruits, and legumes.
5.1.3. Avoid Trigger Foods
Identifying and avoiding trigger foods can help reduce symptoms of soft stool. Common trigger foods include spicy foods, fatty foods, artificial sweeteners, caffeine, and alcohol.
5.1.4. Stay Hydrated
Staying hydrated is essential for maintaining healthy stool consistency. Drink plenty of water, clear broths, and electrolyte-rich beverages to replace fluids lost through soft stool.
5.2. Over-the-Counter Medications
Over-the-counter medications can help relieve symptoms of soft stool, such as diarrhea and abdominal cramps.
5.2.1. Anti-Diarrheal Medications
Anti-diarrheal medications, such as loperamide (Imodium) and bismuth subsalicylate (Pepto-Bismol), can help slow down bowel movements and reduce symptoms of diarrhea. However, these medications should be used with caution, as they can mask symptoms of infection or other underlying conditions.
5.2.2. Probiotics
Probiotics are beneficial bacteria that can help restore the balance of the gut microbiome. Probiotics may help reduce symptoms of soft stool caused by antibiotic use or other disruptions of the gut microbiome.
5.3. Prescription Medications
Prescription medications may be necessary to treat soft stool caused by underlying medical conditions, such as infections or inflammatory bowel disease.
5.3.1. Antibiotics
Antibiotics may be prescribed to treat bacterial infections that are causing soft stool. The specific antibiotic used will depend on the type of bacteria causing the infection.
5.3.2. Anti-Parasitic Medications
Anti-parasitic medications may be prescribed to treat parasitic infections that are causing soft stool. The specific anti-parasitic medication used will depend on the type of parasite causing the infection.
5.3.3. Anti-Inflammatory Medications
Anti-inflammatory medications, such as corticosteroids and aminosalicylates, may be prescribed to treat inflammatory bowel disease (IBD) and reduce symptoms of soft stool and abdominal pain.
5.4. Lifestyle Changes
Making changes to your lifestyle can also help improve stool consistency and reduce symptoms of soft stool.
5.4.1. Manage Stress
Managing stress through relaxation techniques, such as meditation, yoga, or deep breathing exercises, can help reduce stress-related soft stool.
5.4.2. Regular Exercise
Regular exercise can help improve bowel function and reduce symptoms of soft stool. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
5.4.3. Maintain a Regular Sleep Schedule
Maintaining a regular sleep schedule can help regulate bowel function and reduce symptoms of soft stool. Aim for 7-8 hours of sleep per night.
6. When to Seek Medical Attention
While occasional soft stool is usually not a cause for concern, certain symptoms may indicate a more serious underlying condition that requires medical attention.
6.1. Persistent Soft Stool (More Than a Few Days)
If you experience soft stool for more than a few days, it’s important to seek medical attention to determine the underlying cause. Persistent soft stool may be a sign of an infection, inflammatory bowel disease, or other digestive disorder.
6.2. Blood in Stool
Blood in stool, whether it’s bright red or dark and tarry, can be a sign of bleeding in the digestive tract. This symptom requires prompt medical attention to determine the source of the bleeding and receive appropriate treatment.
6.3. Severe Abdominal Pain
Severe abdominal pain, especially if it’s accompanied by other symptoms such as fever, nausea, or vomiting, may indicate a serious digestive problem, such as appendicitis or bowel obstruction.
6.4. High Fever
A high fever (over 101°F or 38.3°C) may indicate an infection that requires medical treatment. If you have a high fever along with soft stool, seek medical attention promptly.
6.5. Dehydration
Dehydration can occur as a result of soft stool, especially if you are experiencing frequent bowel movements. Symptoms of dehydration include thirst, dizziness, fatigue, and decreased urination. If you suspect you are dehydrated, seek medical attention immediately.
6.6. Unexplained Weight Loss
Unexplained weight loss, especially if it’s accompanied by soft stool and other digestive symptoms, may indicate an underlying medical condition, such as inflammatory bowel disease or malabsorption.
7. Preventing Soft Stool
Preventing soft stool involves making lifestyle choices that promote healthy digestion and bowel function.
7.1. Maintain a Balanced Diet
Eating a balanced diet that is rich in fiber, fruits, vegetables, and whole grains can help promote healthy bowel movements and prevent soft stool.
7.2. Stay Hydrated
Drinking plenty of water throughout the day can help maintain healthy stool consistency and prevent dehydration.
7.3. Practice Good Hygiene
Practicing good hygiene, such as washing your hands thoroughly and avoiding contaminated food and water, can help prevent infections that can cause soft stool.
7.4. Manage Stress
Managing stress through relaxation techniques, such as meditation, yoga, or deep breathing exercises, can help prevent stress-related soft stool.
7.5. Limit Alcohol and Caffeine Intake
Limiting alcohol and caffeine intake can help prevent digestive upset and soft stool.
8. Expert Insights on Soft Stool
To provide you with expert insights, we’ve consulted with leading gastroenterologists and digestive health specialists to gather their perspectives on soft stool.
8.1. Dr. Emily Carter, Gastroenterologist
“Soft stool is a common complaint that can often be managed with simple dietary and lifestyle changes. However, persistent soft stool should always be evaluated by a healthcare professional to rule out any underlying medical conditions.”
8.2. Dr. David Miller, Digestive Health Specialist
“The Bristol Stool Chart is a valuable tool for patients to describe their bowel movements and help healthcare providers assess digestive health. Understanding your stool consistency can provide important clues about your overall health.”
8.3. Sarah Johnson, Registered Dietitian
“Fiber is essential for digestive health, but it’s important to increase your fiber intake gradually to avoid digestive upset. Aim for a balanced diet that includes both soluble and insoluble fiber.”
9. Real-Life Stories: Managing Soft Stool
Hearing real-life stories from individuals who have successfully managed soft stool can provide valuable insights and inspiration.
9.1. Maria’s Story
“I struggled with soft stool for years due to lactose intolerance. Once I eliminated dairy from my diet, my symptoms improved dramatically.”
9.2. John’s Story
“Stress was a major trigger for my soft stool. Practicing mindfulness and meditation helped me manage my stress levels and improve my digestive health.”
9.3. Lisa’s Story
“I had persistent soft stool due to an infection. After taking antibiotics and following a bland diet, my symptoms resolved completely.”
10. Addressing Specific Concerns About Soft Stool
Addressing specific concerns about soft stool can help you understand your symptoms and take appropriate action.
10.1. Soft Stool After Eating
Soft stool after eating may be caused by the gastrocolic reflex, a normal physiological response that stimulates bowel movements after a meal. However, if you frequently experience soft stool after eating, it may be a sign of food sensitivity or other digestive disorder.
10.2. Soft Stool in the Morning
Soft stool in the morning may be caused by increased bowel motility during sleep. However, if you consistently experience soft stool in the morning, it may be a sign of underlying digestive issues.
10.3. Soft Stool and Gas
Soft stool and gas are common symptoms that may be caused by bacterial fermentation of undigested food in the intestines. This can be caused by dietary factors, infections, or digestive disorders.
10.4. Soft Stool and Weight Loss
Soft stool and weight loss may indicate malabsorption or other digestive disorders. If you experience unexplained weight loss along with soft stool, it’s important to seek medical attention.
10.5. Soft Stool During Pregnancy
Soft stool during pregnancy is common due to hormonal changes and increased pressure on the digestive system. However, if you experience severe or persistent soft stool during pregnancy, consult your healthcare provider.
11. Soft Stool FAQs
Here are some frequently asked questions about soft stool, along with detailed answers to help you better understand this common digestive issue.
11.1. Is it normal to have soft stool sometimes?
Yes, it is normal to have soft stool occasionally. Temporary changes in diet, stress, or mild infections can cause soft stool that resolves within a few days.
11.2. What does soft stool indicate?
Soft stool can indicate a variety of issues, ranging from dietary factors to underlying medical conditions. Common causes include high-fiber intake, spicy foods, infections, medications, and stress.
11.3. How can I firm up my stool quickly?
To firm up your stool quickly, try following the BRAT diet (bananas, rice, applesauce, toast), increasing your soluble fiber intake, and staying hydrated.
11.4. When should I see a doctor for soft stool?
You should see a doctor for soft stool if you experience persistent symptoms (more than a few days), blood in stool, severe abdominal pain, high fever, dehydration, or unexplained weight loss.
11.5. Can stress cause soft stool?
Yes, stress can cause soft stool. Stress can affect the digestive system by increasing gut motility and altering the balance of gut bacteria.
11.6. Are probiotics helpful for soft stool?
Probiotics may be helpful for soft stool, especially if it is caused by antibiotic use or other disruptions of the gut microbiome. Probiotics can help restore the balance of beneficial bacteria in the intestines.
11.7. What foods should I avoid if I have soft stool?
If you have soft stool, you should avoid trigger foods such as spicy foods, fatty foods, artificial sweeteners, caffeine, and alcohol.
11.8. Can medications cause soft stool?
Yes, certain medications can cause soft stool as a side effect. Common medications that can cause soft stool include antibiotics, laxatives, antacids containing magnesium, and chemotherapy drugs.
11.9. How can I prevent soft stool?
You can prevent soft stool by maintaining a balanced diet, staying hydrated, practicing good hygiene, managing stress, and limiting alcohol and caffeine intake.
11.10. What is the Bristol Stool Chart?
The Bristol Stool Chart is a visual aid used to classify the form of human feces into seven categories, ranging from hard, separate lumps to entirely liquid stool. This chart can help patients describe their bowel movements and assist healthcare professionals in assessing digestive health.
12. Conclusion: Taking Control of Your Digestive Health
Experiencing soft stool can be uncomfortable and concerning, but understanding the potential causes and available solutions can empower you to take control of your digestive health. By making informed dietary choices, managing stress, and seeking appropriate medical attention when needed, you can effectively address soft stool and improve your overall well-being. Remember, consistent and healthy bowel movements are a key indicator of a well-functioning digestive system, and addressing any changes promptly can help maintain optimal health.
Are you still seeking answers and expert advice about your digestive health? At WHY.EDU.VN, we’re dedicated to providing you with reliable and comprehensive information. If you have more questions or need personalized guidance, don’t hesitate to reach out to our team of experts. Contact us at 101 Curiosity Lane, Answer Town, CA 90210, United States, or connect with us via WhatsApp at +1 (213) 555-0101. You can also explore our website, why.edu.vn, to discover a wealth of knowledge and resources to support your journey toward better digestive health. Your well-being is our priority, and we’re here to help you every step of the way.
