Experiencing pain in your vagina can be concerning and uncomfortable. It’s a sensation that many women encounter at some point in their lives, and while it can be alarming, it’s important to know that you are not alone and help is available. Vaginal pain can stem from a variety of causes, ranging from simple irritations to more complex medical conditions. Understanding the potential reasons behind this pain is the first step towards finding relief and ensuring your well-being.
To clarify, when we talk about vaginal pain, it’s helpful to understand the anatomy of the female genitalia. The vagina is the internal muscular canal connecting the uterus to the outside of the body. The vulva, on the other hand, refers to the external parts, including the labia (inner and outer lips), clitoris, the opening of the urethra (where urine exits), and the vaginal opening itself. Pain can occur in either the vagina, the vulva, or both simultaneously.
If your discomfort is located outside these areas but still within the pelvic region – the area below your belly button and above your legs – it might be related to broader pelvic pain issues. However, this article will focus specifically on vaginal and vulval pain. Let’s explore some of the common culprits behind vaginal pain, how to distinguish between them, and most importantly, what you can do to address them and when it’s crucial to seek professional medical advice.
Common Reasons for Vaginal Pain
Vaginal pain is a broad symptom that can manifest in different ways, such as burning, aching, stinging, or throbbing. Pinpointing the exact cause is essential for effective treatment. Here are several common reasons why you might be experiencing vaginal pain:
Vulval Irritation
One of the most frequent causes of discomfort in the vaginal area is vulval irritation. The skin of the vulva is incredibly delicate and sensitive, making it prone to irritation from various everyday factors. Symptoms of vulval irritation often include itching, general discomfort, and a burning sensation.
Common triggers for vulval irritation are:
- Sweating: Moisture and friction from sweat, especially during exercise or hot weather, can irritate the vulval skin.
- Tight Clothing: Wearing tight pants, leggings, or underwear can restrict airflow and cause friction, leading to irritation.
- Eczema or Dermatitis: These skin conditions can affect the vulva, causing dryness, itching, and inflammation.
- Personal Hygiene Products: Certain soaps, douches, wipes, and feminine hygiene sprays can contain harsh chemicals that irritate the sensitive vulval skin.
- Product Allergies: Allergic reactions to laundry detergents, fabric softeners, or even ingredients in condoms or lubricants can cause vulval irritation.
- Infections: As we’ll discuss further, certain infections can initially manifest as vulval irritation.
- Skin Conditions: Conditions like lichen sclerosus can cause chronic vulval irritation and pain.
Dr. Elizabeth Farrell, a gynaecologist and medical director, explains that irritated vulval skin may appear red, swollen, or even cracked. It can also be accompanied by vaginal discharge or general inflammation.
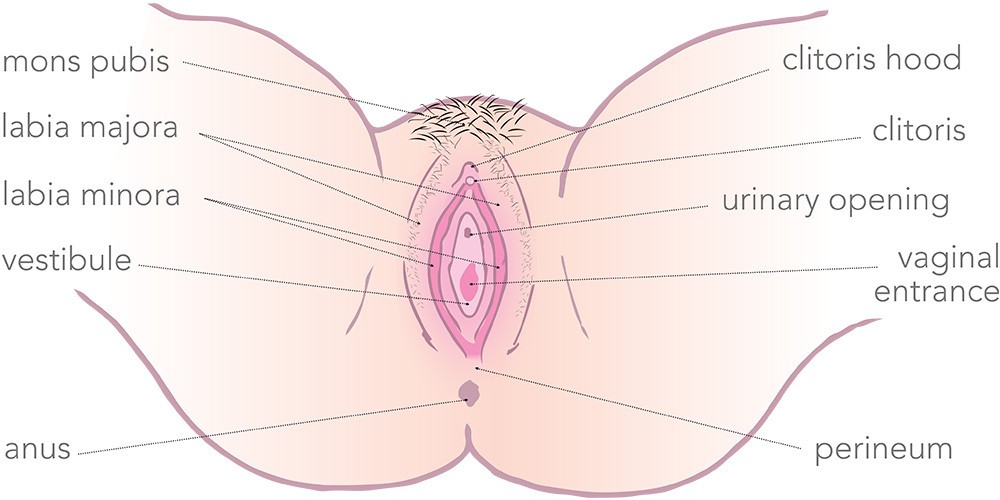 Diagram of the Vulva
Diagram of the Vulva
Alt text: Diagram illustrating the anatomy of the vulva, highlighting key components such as the labia majora and minora, clitoris, urethral opening, and vaginal opening, essential for understanding causes of vulval and vaginal pain.
While vulval irritation is common and often manageable, Dr. Farrell emphasizes the importance of consulting your General Practitioner (GP). A proper examination is necessary to accurately diagnose the cause of the irritation. Often, simple lifestyle adjustments and gentle vulval care practices can alleviate the issue, but the specific treatment will depend on the underlying diagnosis.
Infections
Infections are another significant category of causes for vaginal and vulval pain, often accompanied by a sensation of heat and inflammation.
- Candida (Thrush): This common fungal infection is characterized by inflammation and swelling of the vulva, intense itching, and typically a thick, white discharge resembling cottage cheese. It’s crucial to remember, as Dr. Farrell points out, that “not all itch is thrush.” Self-treating with over-the-counter medications without proper diagnosis can be misleading, and it’s always best to confirm with a GP.
- Bacterial Vaginosis (BV): BV is another prevalent infection caused by an imbalance of bacteria in the vagina. Symptoms include a watery, white, or greenish-grey vaginal discharge, a distinct fishy odor, and sometimes vulval or vaginal pain.
Seeking medical advice is crucial for diagnosing and treating these infections effectively. Prescription medications are often required to clear up infections like thrush and BV and prevent recurrence.
Sexually Transmitted Infections (STIs)
STIs are a significant concern when considering vaginal and vulval pain. Infections like gonorrhoea, chlamydia, trichomoniasis, and herpes can all cause pain in these areas.
However, it’s vital to be aware that some STIs, particularly in their early stages, can be painless or even asymptomatic. Dr. Farrell stresses that “some STIs such as chlamydia can be silent with no symptoms.” Untreated STIs can lead to serious complications, including pelvic inflammatory disease (PID). PID can cause chronic vaginal and pelvic pain and can result in permanent damage to the reproductive system, potentially leading to infertility.
Regular sexual health check-ups are essential, especially when you have a new sexual partner or multiple partners. Practicing safe sex by using condoms consistently can significantly reduce the risk of STIs. Many STIs are easily treatable with antibiotics or antiviral medications when diagnosed promptly.
Vaginismus
Vaginismus is a condition where the pelvic floor muscles involuntarily tighten excessively, narrowing the vaginal opening. This tightening is often associated with anticipated or actual vaginal penetration, such as during sexual intercourse.
Dr. Farrell explains that vaginismus is strongly linked to painful sexual experiences and, in some cases, can make any form of vaginal penetration impossible. Women with vaginismus may also experience pain or difficulty when using tampons or menstrual cups, or during pelvic examinations like cervical screening tests, which can become extremely painful or impossible to perform.
Vaginismus is a complex condition that often requires a multidisciplinary approach to treatment. This typically involves a team of healthcare professionals, including a compassionate GP, a pelvic floor physiotherapist to teach muscle relaxation techniques, and a psychologist to address any underlying psychological factors contributing to the condition.
Vulval/Vaginal Dryness
Dryness in the vulval and vaginal areas can occur at any age but is particularly common after menopause. This is primarily due to a natural decrease in oestrogen levels during menopause. Oestrogen plays a vital role in maintaining the moisture and thickness of vaginal tissues. When oestrogen levels decline, these tissues can become thinner, drier, and more vulnerable to damage and irritation.
Dr. Farrell describes the sensation of sex after menopause, without sufficient lubrication, as feeling like “sandpaper.” Reduced lubrication can also result from other hormonal shifts, such as those experienced during breastfeeding.
While vaginal dryness can be a natural part of hormonal changes, persistent pain or discomfort should be addressed. Using a good-quality personal lubricant during sexual activity can significantly alleviate dryness-related pain. Water-based lubricants are generally recommended, and petroleum jelly should be avoided as it can damage condoms and diaphragms. If dryness persists or worsens despite using lubricants, consulting your GP is advisable as there are effective treatments available, including topical oestrogen creams or pessaries.
Vulvodynia
Vulvodynia is a chronic pain condition characterized by persistent, unexplained pain in the vulva. The pain is often described as burning, stinging, or raw, and can be localized to a specific area or spread across the entire vulva.
A key characteristic of vulvodynia is that the pain cannot be attributed to any identifiable infection, skin condition, or other visible cause. The pain may be constant or intermittent and can be triggered by touch (provoked vulvodynia) or occur spontaneously (unprovoked vulvodynia). Provoked vulvodynia refers to pain triggered by pressure or touch, such as tampon insertion, sexual intercourse, or even prolonged sitting. Unprovoked vulvodynia is characterized by pain that is present without any apparent trigger.
Dr. Farrell emphasizes that women with vulvodynia typically have a “normal-looking vulva,” meaning there are no visible signs of irritation, inflammation, or disease. Vulvodynia is a chronic condition that can persist for months or years, significantly impacting a woman’s quality of life. However, it is treatable, often requiring a multidisciplinary team of healthcare professionals to manage the pain effectively.
Lichen Sclerosus
Lichen sclerosus is a chronic inflammatory skin condition that most commonly affects the vulva and the skin around the anus, although it can occur in other areas of the body. It can affect women of all ages, but it is most prevalent in postmenopausal women.
Lichen sclerosus causes patches of skin in the affected areas to become white, thinned, and sometimes crinkled. These patches can be intensely itchy and painful. Over time, lichen sclerosus can lead to permanent changes in the vulval anatomy, such as the shrinking and fusion of the labia minora (inner lips), known as adhesions.
The exact cause of lichen sclerosus remains unknown, but it is believed to be an autoimmune condition, where the body’s immune system mistakenly attacks healthy tissues. Women with lichen sclerosus have a slightly increased risk of developing vulvar cancer, making long-term monitoring and management of this condition essential.
Vaginal Tears and Procedures During Childbirth
Childbirth is a common cause of vaginal pain, particularly due to vaginal tears that occur during delivery. The severity of these tears varies. Minor tears may heal naturally, while more significant tears require stitches.
Episiotomies, surgical incisions made to enlarge the vaginal opening during childbirth, are also a common procedure. Episiotomies are typically performed when the baby needs to be delivered quickly due to distress or if forceps or vacuum extraction is necessary. Episiotomies always require stitches for repair.
Recovery from vaginal tears or episiotomy repairs involves healing, which can cause pain and discomfort. Pain medication, such as paracetamol, is often recommended during the initial recovery period. Dr. Farrell notes that this pain is normal and should subside as the tissues heal. However, it is essential to be vigilant for signs of infection, such as increasing pain, swelling around the stitches, or a foul odor, which require immediate medical attention.
Persistent Pelvic Pain
Persistent pelvic pain, a chronic pain condition in the pelvic region, can sometimes contribute to or exacerbate vulval and vaginal pain. This can occur due to overactive pelvic floor muscles, vulvodynia, or a combination of both conditions. Managing persistent pelvic pain often requires a comprehensive approach addressing both the underlying pelvic pain and the associated vaginal symptoms.
Key Advice for Women with Vaginal or Vulval Pain
Navigating vaginal or vulval pain can be daunting, but remember these crucial points:
- You don’t have to suffer in silence. Pain in this area is a valid health concern and not something to be embarrassed or ashamed about. Pain is a signal from your body that something needs attention. Listen to it and seek answers.
- Get an expert opinion. Vaginal and vulval pain can vary greatly in intensity and duration and can be caused by a wide spectrum of conditions, some less serious than others. Visiting your GP is the most important first step. They can conduct a thorough examination to diagnose your specific condition accurately and ensure you receive the correct treatment. If you feel unheard or uncomfortable with your current GP, consider seeking a women’s health clinic, a gynaecologist, or a sexual health clinic with specialized expertise in this area.
- Know what’s normal for you. Familiarity with your own body is key to recognizing when something is amiss. Everyone’s body is unique, and there is no single “normal.” Understanding your own baseline makes it easier to identify changes and seek help when needed.
- Be wary of home remedies. The internet can be tempting for quick solutions, but it’s crucial to prioritize evidence-based health advice from reliable sources. Avoid douching and vaginal steaming, as these practices can disrupt the natural vaginal balance and potentially worsen irritation. Always consult your doctor before using any non-medical treatments on your vulva or vagina. They may recommend specific over-the-counter products from a pharmacy if appropriate.
- Know that help, support, and treatment are available. Vulval and vaginal pain can be complex and impact various aspects of life, from self-esteem and physical comfort to sexual relationships and daily activities. Seeking specialized care from healthcare professionals like skin specialists, pelvic floor physiotherapists, psychologists, or sex therapists can make a significant positive difference in managing and overcoming vaginal pain.
Remember, you don’t have to live with vaginal pain. Seeking timely and appropriate medical advice is the most empowering step you can take towards understanding the cause of your discomfort and finding effective relief.