Why Does My Knee Hurt When It Rains, you might wonder? Rainy days can bring more than just wet weather; for many, they also bring joint discomfort. At WHY.EDU.VN, we explore this connection, offering insights into weather-related knee pain and potential relief strategies. Let’s delve into the correlation between barometric pressure, joint pain, and atmospheric changes to provide a comprehensive overview. We’ll also touch upon arthritis pain and seasonal discomfort, addressing your concerns effectively.
1. The Age-Old Question: Does Weather Really Affect Knee Pain?
It’s a common belief: “I can feel it in my bones when it’s going to rain.” But is there any truth to this? Many people with arthritis or other joint conditions swear that their pain worsens with changes in the weather. A significant percentage, around 67%, of individuals with osteoarthritis in their knees, hips, or hands report that weather influences their pain levels.[1] This observation begs the question: Is this just an old wives’ tale, or is there a scientific basis for this phenomenon?
2. Unraveling the Mystery: The Science Behind Weather-Related Joint Pain
While anecdotal evidence is abundant, scientific research has yielded mixed results regarding the direct link between weather and knee pain. There are typically three main weather factors believed to play a role in knee discomfort: temperature, humidity, and atmospheric pressure changes associated with rain.
- Inconsistent Findings: A comprehensive review of studies examining the relationship between these weather variables and arthritic pain has shown inconsistent results.[2] Some studies found no connection at all, while others indicated a correlation with one or more weather aspects.
- Common Associations: When a link was identified, it often involved cold temperatures, high humidity, and low barometric pressure. However, some studies even reported the opposite effect, further complicating the picture.
- Individual Sensitivity: Despite the conflicting findings, one consistent observation emerges: some individuals with osteoarthritis are indeed “weather-sensitive.” This means that changes in weather conditions trigger increased pain levels for them, while others remain unaffected. Rain and other weather changes appear to be linked to knee pain in some people, but not in others. It depends on the individual.
3. Decoding the Weather’s Impact: How Different Factors Contribute to Knee Pain
While the exact mechanisms are still under investigation, here are some of the prevailing theories explaining how specific weather changes might exacerbate knee pain in individuals with osteoarthritis:
3.1. Rain and Atmospheric Pressure Changes
It’s not the rain itself, but the change in atmospheric pressure associated with it, that is often implicated in increased knee pain.
- The Theory: In people with knee osteoarthritis, the protective cartilage and other tissues surrounding the knee joint are damaged, exposing pressure-sensing nerve endings. This heightened sensitivity makes these nerves more reactive to the pressure fluctuations that occur before and during rainfall.[3]
- Expansion and Contraction: Another theory suggests that changes in atmospheric pressure can cause damaged tissues within the knee to expand and contract, leading to discomfort and pain.[4]
3.2. Cold Temperatures
Cold weather is another commonly cited culprit for increased knee pain.
- The Theory: The synovial fluid within and around the knee joint acts as a lubricant, enabling smooth and pain-free movement. Cold temperatures may cause this fluid to thicken, resulting in a stiffer joint and increased friction between joint surfaces, leading to pain.
- Muscle and Tendon Effects: Cold weather can also affect the contractibility and elasticity of muscles and tendons surrounding the knee joint, further contributing to pain and stiffness.[3]
3.3. Humidity
Humidity’s role in knee pain is also a subject of debate and individual variation.
- The Theory: High humidity is believed to cause damaged and inflamed tissues within the knee joint to expand, further reducing the space within the joint and increasing pain.
- Dry Weather Relief: Conversely, dry weather may allow these tissues to relax, creating more space in the joint and facilitating easier, less painful movement. However, it’s crucial to remember that this is just a theory, and relocating to a drier climate won’t necessarily alleviate knee pain.
3.4. The Psychological Impact of Bad Weather
It’s essential not to overlook the psychological impact of bad weather on pain perception.
- Mood and Pain: Studies have shown that bad weather can negatively affect mood, which, in turn, can influence how much pain a person experiences.[3]
- Reduced Activity: Rainy days often lead to decreased physical activity and increased time spent indoors. Staying active is crucial for managing osteoarthritis pain, so prolonged inactivity due to bad weather can exacerbate discomfort.[5]
Table 1: Weather Factors and Their Potential Impact on Knee Pain
| Weather Factor | Potential Mechanism |
|---|---|
| Atmospheric Pressure | Changes cause expansion/contraction of tissues, stimulating exposed nerve endings. |
| Cold Temperatures | Thickens synovial fluid, increasing friction; affects muscle and tendon elasticity. |
| High Humidity | Causes tissue expansion, reducing joint space and increasing pressure. |
| Bad Weather Mood | Negative mood impacts pain perception; reduces physical activity, increasing stiffness and pain. |
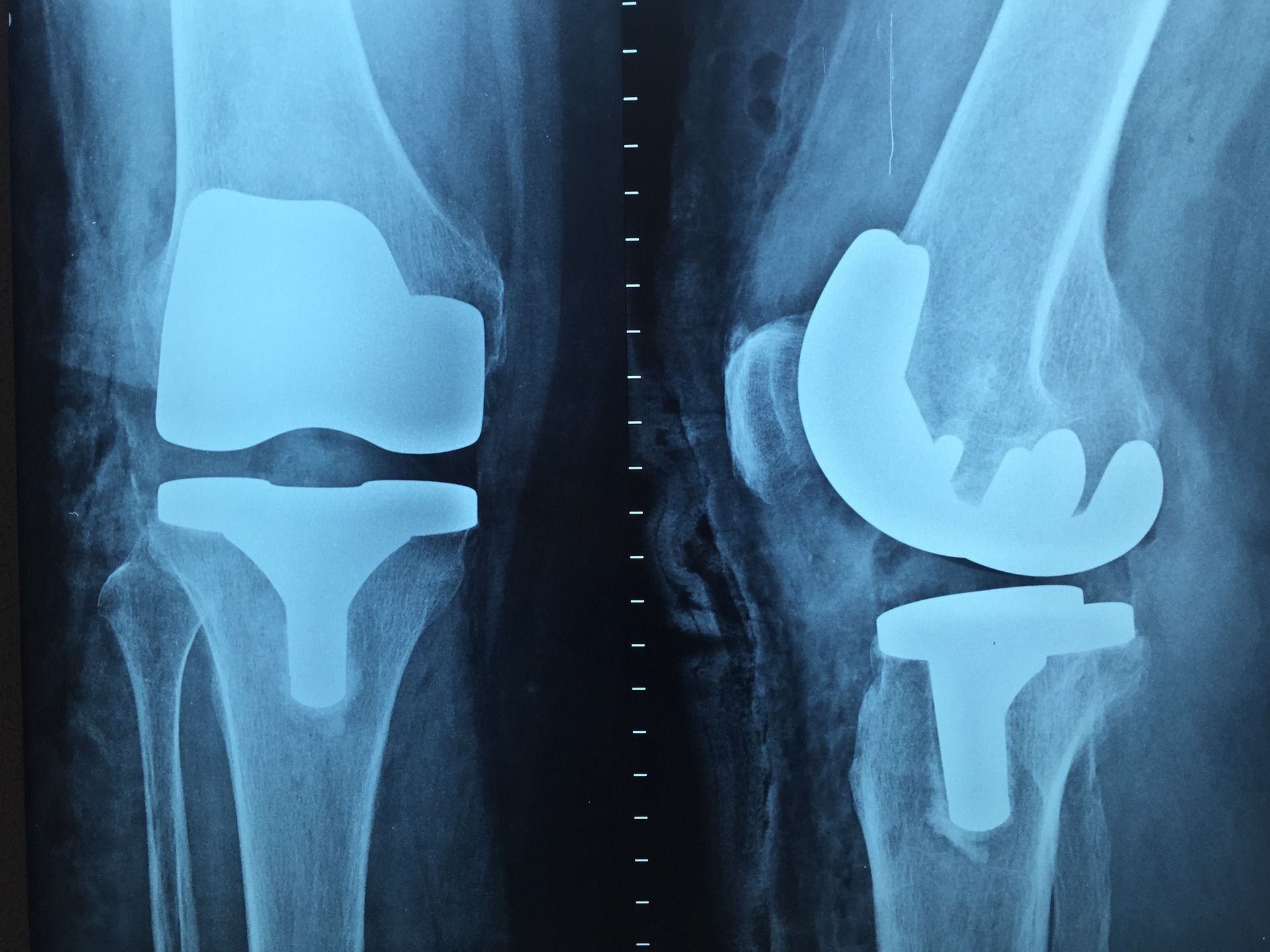


4. Knee Replacement and Weather Sensitivity: What to Expect
If you’ve undergone a knee replacement, you might wonder if it will eliminate weather-related knee pain.
- Knee Replacement Goals: A knee replacement aims to reduce pain and improve mobility in individuals with osteoarthritis. Physical therapy following surgery can significantly decrease pain and enhance quality of life.[6]
- Potential for Lingering Sensitivity: However, some individuals may still experience pain or stiffness in their knee during rainy weather even after a replacement. This could be because a knee replacement addresses the symptoms of osteoarthritis but doesn’t cure the underlying disease.
- Weight and Sensations: Additionally, a replaced knee may feel heavier and different, potentially making it more sensitive to weather changes.
Despite these factors, the goal is that the overall reduction in pain achieved through knee replacement and physical therapy will also translate to less weather-related knee discomfort.[[6]](#footnote6]
5. Practical Tips for Managing Weather-Related Knee Pain
While you can’t control the weather, you can take steps to manage your knee pain and minimize the impact of weather changes:
5.1. Stay Active, Regardless of the Weather
Regular exercise is crucial for managing osteoarthritis pain. Aim for a mix of:
- Strengthening exercises: To build muscle support around the knee.
- Range-of-motion exercises: To maintain flexibility.
- Aerobic exercises: Like walking or swimming, to improve overall fitness.
Even on rainy days, try to find ways to stay active indoors, such as:
- Walking around your home
- Using a stationary bike
- Following a workout video
- Practicing yoga or tai chi
5.2. Keep Warm
Cold weather can exacerbate knee pain, so dress warmly, especially during the winter months. Consider:
- Wearing layers of clothing
- Using knee warmers or braces
- Taking warm baths or showers
5.3. Manage Your Mood
Bad weather can negatively impact your mood, so make an effort to stay positive and engaged. Try:
- Spending time with loved ones
- Engaging in hobbies you enjoy
- Practicing relaxation techniques like meditation or deep breathing
- Seeking professional help if you’re struggling with depression or anxiety
5.4. Monitor and Track Your Pain
Keep a journal or use a pain-tracking app to monitor your pain levels and identify any patterns related to weather changes. This information can help you:
- Anticipate when your pain might worsen
- Adjust your activities accordingly
- Communicate effectively with your doctor or physical therapist
5.5. Consult With a Healthcare Professional
If your weather-related knee pain is significantly impacting your quality of life, it’s essential to seek professional medical advice. A doctor or physical therapist can:
- Diagnose the underlying cause of your pain
- Recommend appropriate treatment options
- Provide personalized advice on managing your condition
Table 2: Strategies for Managing Weather-Related Knee Pain
| Strategy | Description |
|---|---|
| Stay Active | Regular exercise improves joint health and reduces pain; find indoor activities on bad weather days. |
| Keep Warm | Dress in layers, use knee warmers, and take warm baths to combat cold-related stiffness and pain. |
| Manage Mood | Engage in enjoyable activities, practice relaxation techniques, and seek help if needed to maintain a positive outlook. |
| Monitor Pain | Track pain levels and weather conditions to identify triggers and patterns, helping anticipate and manage pain effectively. |
| Consult a Professional | Seek medical advice for diagnosis, treatment options, and personalized management strategies for persistent or severe weather-related pain. |
6. Debunking Myths and Addressing Common Concerns
Let’s address some common myths and concerns related to weather-related knee pain:
- Myth: It’s all in your head. While psychological factors can play a role, the connection between weather and joint pain is a real phenomenon experienced by many individuals with osteoarthritis.
- Concern: Moving to a warmer climate will cure my pain. While some individuals find relief in warmer, drier climates, this is not a guaranteed solution, and the effects can vary significantly from person to person.
- Myth: There’s nothing you can do about weather-related pain. While you can’t control the weather, there are numerous strategies you can employ to manage your pain and minimize its impact on your daily life.
7. Exploring Advanced Treatment Options
In addition to the self-management strategies mentioned above, several advanced treatment options are available for individuals with severe or persistent weather-related knee pain:
- Medications: Pain relievers, anti-inflammatory drugs, and other medications can help manage pain and inflammation.
- Injections: Corticosteroid injections can provide temporary pain relief by reducing inflammation within the joint.
- Physical Therapy: A physical therapist can develop a personalized exercise program to strengthen muscles, improve flexibility, and reduce pain.
- Surgery: In severe cases, joint replacement surgery may be an option to relieve pain and restore function.
8. The Importance of a Holistic Approach
Managing weather-related knee pain often requires a holistic approach that addresses physical, psychological, and lifestyle factors. This may involve:
- Working with a healthcare team: Including a doctor, physical therapist, psychologist, and other specialists.
- Adopting a healthy lifestyle: Including a balanced diet, regular exercise, and stress management techniques.
- Building a strong support system: Connecting with friends, family, and other individuals who understand your condition.
9. The Role of Technology in Pain Management
Technology can play a significant role in managing weather-related knee pain.
- Pain-tracking apps: Can help you monitor your pain levels and identify patterns related to weather changes.
- Weather apps: Can provide you with real-time weather information, allowing you to anticipate when your pain might worsen.
- Online communities: Can connect you with other individuals who share your experiences and offer support and advice.
10. Understanding Different Types of Knee Pain
It’s important to understand that not all knee pain is the same. Different types of knee pain may be caused by different underlying conditions and may respond differently to weather changes. Some common types of knee pain include:
- Osteoarthritis pain: Caused by the breakdown of cartilage in the joint.
- Rheumatoid arthritis pain: Caused by an autoimmune disorder that attacks the joints.
- Patellofemoral pain syndrome: Pain around the kneecap, often caused by overuse or misalignment.
- Meniscus tears: Tears in the cartilage that cushions the knee joint.
- Ligament injuries: Injuries to the ligaments that support the knee joint.
11. The Future of Research: What’s Next in Understanding Weather-Related Pain?
Research into the relationship between weather and pain is ongoing. Future studies may focus on:
- Identifying specific genes: That make individuals more susceptible to weather-related pain.
- Developing more accurate models: To predict the impact of weather changes on pain levels.
- Evaluating the effectiveness of different treatments: For weather-related pain.
- Exploring the role of the brain: In processing and interpreting pain signals in response to weather changes.
12. Additional Factors Contributing to Joint Pain
While weather can certainly play a role, it’s important to remember that other factors can also contribute to joint pain, including:
- Age: Joint pain becomes more common with age as cartilage breaks down and joints become stiffer.
- Weight: Excess weight puts extra stress on joints, increasing the risk of pain and injury.
- Previous injuries: Previous injuries to a joint can increase the risk of developing arthritis and pain later in life.
- Genetics: Some people are genetically predisposed to developing arthritis and joint pain.
- Occupation: Certain occupations that involve repetitive movements or heavy lifting can increase the risk of joint pain.
13. Nutrition and Joint Health: Foods to Eat and Avoid
A healthy diet can play a significant role in managing joint pain. Some foods that may help reduce inflammation and pain include:
- Fatty fish: Rich in omega-3 fatty acids, which have anti-inflammatory properties.
- Fruits and vegetables: Rich in antioxidants and vitamins that support joint health.
- Whole grains: Provide fiber and nutrients that can help reduce inflammation.
- Healthy fats: Like olive oil and avocados, which have anti-inflammatory properties.
Foods to avoid that may worsen inflammation and pain include:
- Processed foods: Often high in sugar, unhealthy fats, and additives that can promote inflammation.
- Red meat: Can contribute to inflammation in some people.
- Sugary drinks: Can promote inflammation and weight gain, which can worsen joint pain.
- Excessive alcohol: Can interfere with medications and worsen inflammation.
14. Alternative Therapies for Knee Pain Relief
Many people find relief from knee pain through alternative therapies, such as:
- Acupuncture: Involves inserting thin needles into specific points on the body to relieve pain.
- Massage therapy: Can help reduce muscle tension and improve circulation.
- Yoga: Can improve flexibility, strength, and balance, which can help reduce knee pain.
- Tai chi: A gentle form of exercise that can improve balance, coordination, and pain management.
- Herbal remedies: Some herbal remedies, such as turmeric and ginger, have anti-inflammatory properties.
15. Understanding Barometric Pressure and Its Effects
Barometric pressure, also known as atmospheric pressure, is the weight of the air surrounding us. Changes in barometric pressure can affect our bodies in several ways, including:
- Joint pain: As discussed earlier, changes in barometric pressure can affect joint pain, especially in people with arthritis.
- Headaches: Some people are sensitive to changes in barometric pressure and may experience headaches or migraines.
- Sinus problems: Changes in barometric pressure can affect the sinuses, causing pain, congestion, and pressure.
- Dizziness: Some people may experience dizziness or lightheadedness with changes in barometric pressure.
16. The Mind-Body Connection and Pain Perception
The mind-body connection plays a significant role in pain perception. Factors such as stress, anxiety, and depression can all amplify pain signals. Techniques such as mindfulness meditation, deep breathing exercises, and cognitive-behavioral therapy can help manage pain by:
- Reducing stress and anxiety
- Improving mood
- Changing thought patterns about pain
- Promoting relaxation
17. Creating a Comfortable Environment for Pain Relief
Creating a comfortable environment can also help manage knee pain. This may involve:
- Using supportive cushions and pillows: To support your knees and joints while sitting or lying down.
- Adjusting your workstation: To ensure proper posture and reduce strain on your joints.
- Using assistive devices: Such as canes or walkers, to reduce stress on your knees.
- Maintaining a comfortable temperature: Avoid extreme temperatures that can worsen pain.
18. The Importance of Early Diagnosis and Intervention
Early diagnosis and intervention are crucial for managing knee pain and preventing long-term damage. If you experience persistent knee pain, it’s important to see a doctor to determine the underlying cause and receive appropriate treatment. Early intervention can help:
- Slow the progression of arthritis
- Prevent further joint damage
- Improve quality of life
19. Staying Informed: Resources for Knee Pain Management
Staying informed about knee pain and its management is essential. Here are some valuable resources:
- The Arthritis Foundation: Provides information, support, and resources for people with arthritis.
- The American Academy of Orthopaedic Surgeons: Offers information on orthopaedic conditions and treatments.
- The National Institute of Arthritis and Musculoskeletal and Skin Diseases: Conducts research and provides information on arthritis and related conditions.
20. Personal Stories: Real-Life Experiences With Weather-Related Pain
Hearing from others who experience weather-related pain can be helpful and validating. Many online communities and support groups provide a platform for sharing personal stories and experiences. Reading these stories can help you feel less alone and provide valuable insights into coping strategies.
21. The Impact of Lifestyle Choices on Joint Health
Your lifestyle choices can significantly impact your joint health. Consider the following:
- Smoking: Smoking can damage cartilage and increase the risk of arthritis.
- Alcohol: Excessive alcohol consumption can interfere with medications and worsen inflammation.
- Sedentary lifestyle: A sedentary lifestyle can lead to muscle weakness and stiffness, which can worsen joint pain.
- Poor posture: Poor posture can put extra stress on your joints, increasing the risk of pain and injury.
22. Seasonal Variations in Knee Pain: Beyond the Rain
While rain is a common trigger, other seasonal variations can also affect knee pain:
- Winter: Cold temperatures can cause stiffness and pain.
- Summer: Heat and humidity can cause swelling and discomfort.
- Spring and Fall: Changes in barometric pressure can trigger pain.
23. Understanding the Inflammatory Response in Joint Pain
Inflammation is a key factor in joint pain. Understanding the inflammatory response can help you manage your pain more effectively. Inflammation is the body’s natural response to injury or infection, but chronic inflammation can damage joints and cause pain. Strategies to reduce inflammation include:
- Anti-inflammatory medications: Such as NSAIDs.
- Dietary changes: Eating a diet rich in anti-inflammatory foods.
- Lifestyle changes: Such as regular exercise and stress management.
24. The Psychological Benefits of Support Groups
Joining a support group can provide numerous psychological benefits for people with knee pain:
- Reduced feelings of isolation: Connecting with others who understand your experiences can help you feel less alone.
- Increased coping skills: Sharing tips and strategies can help you manage your pain more effectively.
- Improved mood: Support groups can provide a sense of community and belonging, which can improve your mood.
- Increased self-esteem: Helping others can boost your self-esteem and sense of purpose.
25. Assistive Devices: Tools for Pain Relief and Mobility
Assistive devices can help relieve pain and improve mobility for people with knee pain:
- Canes: Can provide support and reduce stress on your knees.
- Walkers: Can provide more stability than canes and are helpful for people with significant balance problems.
- Braces: Can provide support and stability to your knees.
- Shoe inserts: Can help align your feet and ankles, reducing stress on your knees.
26. The Role of Sleep in Pain Management
Sleep plays a crucial role in pain management. Lack of sleep can worsen pain and make it more difficult to cope. Aim for 7-8 hours of sleep per night. Strategies to improve sleep include:
- Establishing a regular sleep schedule: Going to bed and waking up at the same time each day.
- Creating a relaxing bedtime routine: Such as taking a warm bath or reading a book.
- Avoiding caffeine and alcohol before bed: These substances can interfere with sleep.
- Creating a comfortable sleep environment: Ensuring your bedroom is dark, quiet, and cool.
27. Understanding the Different Stages of Osteoarthritis
Osteoarthritis progresses through different stages, each with varying levels of pain and joint damage. Understanding the stage of your osteoarthritis can help you and your doctor develop an appropriate treatment plan. The stages of osteoarthritis are typically classified as:
- Stage 0: Normal joint.
- Stage 1: Minor cartilage wear.
- Stage 2: Mild cartilage damage.
- Stage 3: Moderate cartilage damage.
- Stage 4: Severe cartilage damage.
28. The Impact of Exercise on Cartilage Health
While it may seem counterintuitive, exercise can actually improve cartilage health. Low-impact exercises such as swimming, cycling, and walking can help:
- Increase blood flow to the cartilage
- Strengthen the muscles that support the joint
- Reduce inflammation
- Maintain joint flexibility
29. Managing Pain Flare-Ups: Strategies for Immediate Relief
Even with consistent management, pain flare-ups can still occur. Strategies for immediate relief include:
- Rest: Avoid activities that aggravate your pain.
- Ice: Apply ice to the affected area for 15-20 minutes at a time.
- Heat: Apply heat to the affected area for 15-20 minutes at a time.
- Over-the-counter pain relievers: Such as ibuprofen or acetaminophen.
- Topical pain relievers: Such as creams or gels containing menthol or capsaicin.
30. Knee Pain and Weight Management: A Critical Connection
Maintaining a healthy weight is crucial for managing knee pain. Excess weight puts extra stress on your knee joints, increasing the risk of pain and injury. Losing even a small amount of weight can significantly reduce knee pain and improve function. Strategies for weight management include:
- Eating a healthy diet: Focusing on fruits, vegetables, whole grains, and lean protein.
- Regular exercise: Aiming for at least 30 minutes of moderate-intensity exercise most days of the week.
- Working with a registered dietitian: To develop a personalized meal plan.
31. Understanding Viscosupplementation for Knee Pain
Viscosupplementation involves injecting hyaluronic acid into the knee joint. Hyaluronic acid is a naturally occurring substance in the synovial fluid that helps lubricate and cushion the joint. Viscosupplementation can help:
- Reduce pain
- Improve joint function
- Delay the need for joint replacement surgery
32. The Role of Regenerative Medicine in Knee Pain Treatment
Regenerative medicine is a promising field that aims to repair or replace damaged tissues in the body. Some regenerative medicine therapies being explored for knee pain include:
- Platelet-rich plasma (PRP) injections: Involve injecting a concentrated solution of platelets into the knee joint to promote healing.
- Stem cell therapy: Involves injecting stem cells into the knee joint to regenerate damaged cartilage.
33. Exploring the Use of Orthotics for Knee Pain Relief
Orthotics are custom-made shoe inserts that can help align your feet and ankles, reducing stress on your knees. Orthotics can be particularly helpful for people with:
- Flat feet
- High arches
- Uneven leg length
34. Long-Term Management Strategies for Chronic Knee Pain
Chronic knee pain requires a long-term management approach that may involve a combination of strategies. It’s important to work with your healthcare team to develop a personalized plan that addresses your specific needs and goals. Long-term management strategies may include:
- Regular exercise
- Weight management
- Medications
- Physical therapy
- Assistive devices
- Alternative therapies
- Lifestyle modifications
35. The Importance of Self-Care in Pain Management
Self-care is an essential component of pain management. Taking care of your physical, emotional, and mental health can help you cope with pain and improve your overall well-being. Self-care strategies may include:
- Getting enough sleep
- Eating a healthy diet
- Regular exercise
- Stress management
- Spending time with loved ones
- Engaging in hobbies you enjoy
- Practicing mindfulness and meditation
36. Understanding the Impact of Knee Pain on Mental Health
Knee pain can have a significant impact on mental health. Chronic pain can lead to:
- Depression
- Anxiety
- Irritability
- Sleep disturbances
- Social isolation
It’s important to address the psychological effects of knee pain and seek professional help if needed.
37. Empowering Yourself: Taking Control of Your Knee Pain Journey
Living with knee pain can be challenging, but it’s important to remember that you are not alone. By staying informed, working with your healthcare team, and adopting a proactive approach to pain management, you can empower yourself and take control of your knee pain journey.
38. When Is It Time to Consider Knee Replacement Surgery?
Knee replacement surgery is a significant decision, and it’s important to consider all of your options before proceeding. Knee replacement surgery may be an option if:
- You have severe knee pain that interferes with your daily activities.
- Non-surgical treatments have not provided adequate relief.
- You have significant joint damage.
- Your quality of life is significantly impacted by your knee pain.
39. Frequently Asked Questions (FAQs) About Weather-Related Knee Pain
Q1: Why does my knee hurt more when it rains?
A: Changes in barometric pressure associated with rain can cause tissues in the knee joint to expand and contract, irritating nerve endings.
Q2: Does cold weather really make knee pain worse?
A: Yes, cold temperatures can cause the fluid in the knee joint to thicken, leading to stiffness and pain.
Q3: Can humidity affect knee pain?
A: High humidity may cause tissues in the knee joint to expand, increasing pressure and pain.
Q4: Is there anything I can do to prevent weather-related knee pain?
A: While you can’t prevent weather changes, you can manage your pain with exercise, warmth, and mood management.
Q5: Will a knee replacement eliminate weather-related pain?
A: It may reduce pain, but some individuals still experience sensitivity due to underlying conditions.
Q6: Are there any specific exercises that help with knee pain?
A: Low-impact exercises like swimming, walking, and cycling are beneficial.
Q7: Can my diet affect my knee pain?
A: Yes, a diet rich in anti-inflammatory foods can help reduce pain.
Q8: Is it normal for my knee to hurt more on certain days?
A: Yes, weather changes can cause fluctuations in pain levels.
Q9: Should I see a doctor for my knee pain?
A: If your pain is persistent and affects your daily life, consult a healthcare professional.
Q10: Are there any alternative therapies that can help with knee pain?
A: Acupuncture, massage therapy, and yoga may provide relief.
40. WHY.EDU.VN: Your Partner in Understanding and Managing Knee Pain
At WHY.EDU.VN, we understand the challenges of living with knee pain. Our mission is to provide you with accurate, reliable, and easy-to-understand information to help you manage your condition and improve your quality of life. Visit our website at WHY.EDU.VN to find answers to your questions, connect with experts, and discover resources to support your journey.
Don’t let knee pain control your life. Let WHY.EDU.VN be your guide to understanding and managing your pain. We offer a wealth of information and resources to help you take control of your health and well-being. Have a specific question? Our experts are ready to provide personalized answers and guidance. Visit us at 101 Curiosity Lane, Answer Town, CA 90210, United States, or contact us via Whatsapp at +1 (213) 555-0101. Visit why.edu.vn today and start your journey to a pain-free life! We provide answers, promote well-being, and offer practical guidance.
References
[1] Timmermans EJ, van der Pas S, Schaap LA, et al. Self-perceived weather sensitivity and joint pain in older people with osteoarthritis in six European countries: results from the European Project on OSteoArthritis (EPOSA). BMC Musculoskelet Disord. 2014;15:66. doi:10.1186/1471-2474-15-66
[2] Smedslund G, Hagen KB. Does rain really cause pain? A systematic review of the associations between weather factors and severity of pain in people with rheumatoid arthritis. Eur J Pain. 2011;15(1):5-10. doi:10.1016/j.ejpain.2010.05.003
[3] Timmermans EJ, Schaap LA, Herbolsheimer F, et al. The Influence of Weather Conditions on Joint Pain in Older People with Osteoarthritis: Results from the European Project on OSteoArthritis. J Rheumatol. 2015;42(10):1885-1892. doi:10.3899/jrheum.141594
[4] Jamison RN, Anderson KO, Slater MA. Weather changes and pain: perceived influence of local climate on pain complaint in chronic pain patients. Pain. 1995;61(2):309-315. doi:10.1016/0304-3959(94)00215-Z
[5] Fu K, Metcalf B, Bennell KL, et al. Association of weather factors with the risk of pain exacerbations in people with hip osteoarthritis. Scand J Rheumatol. 2021;50(1):68-73. doi:10.1080/03009742.2020.1760929
[6] Bade MJ, Kohrt WM, Stevens-Lapsley JE. Outcomes before and after total knee arthroplasty compared to healthy adults. J Orthop Sports Phys Ther. 2010;40(9):559-567. doi:10.2519/jospt.2010.3317