Why Does My Ball Hurt? If you are experiencing discomfort in your testicle, it could stem from a variety of causes, but often it’s related to a condition called varicocele. At WHY.EDU.VN, we aim to provide you with accurate information and potential solutions to ease your concerns. Recognizing the source of the discomfort and seeking appropriate care is crucial for your overall health and well-being, and we can help you explore the possibilities, including testicular pain management and scrotal discomfort remedies.
1. Common Causes of Testicular Pain
Testicular pain, also known as scrotal pain, can arise from a variety of factors, ranging from minor injuries to more significant medical conditions. Understanding the potential causes is the first step in seeking appropriate care and finding relief. Here’s an overview of some of the common culprits behind testicular discomfort:
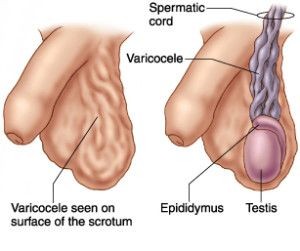
1.1. Varicocele
Varicocele is one of the most frequent causes of chronic testicular pain, affecting approximately 15% of adult men. It involves the enlargement of veins within the scrotum, similar to varicose veins in the legs. This condition can cause a dull, aching pain that worsens with standing or physical activity and improves when lying down.
1.2. Epididymitis
Epididymitis is an inflammation of the epididymis, a coiled tube at the back of the testicle that stores and carries sperm. This condition is often caused by a bacterial infection, including sexually transmitted infections (STIs) like chlamydia and gonorrhea. Symptoms typically include testicular pain, swelling, redness, and warmth in the scrotum.
1.3. Testicular Torsion
Testicular torsion is a medical emergency that occurs when the testicle rotates, twisting the spermatic cord and cutting off blood supply. This condition causes sudden, severe testicular pain, often accompanied by nausea, vomiting, and swelling. Testicular torsion requires immediate medical attention to prevent permanent damage to the testicle. The viability of the testicle decreases rapidly after about six hours of torsion.
1.4. Hydrocele
A hydrocele is a fluid-filled sac surrounding a testicle, causing swelling in the scrotum. While hydroceles are usually painless, they can cause discomfort or a feeling of heaviness in the scrotum, especially as they increase in size.
1.5. Testicular Cancer
Although less common, testicular cancer can sometimes manifest as testicular pain or discomfort. Other symptoms may include a lump in the testicle, swelling, or a feeling of heaviness in the scrotum. Early detection and treatment are crucial for successful outcomes with testicular cancer.
1.6. Trauma or Injury
Direct trauma to the testicles, such as from a sports injury or accident, can cause immediate and intense pain. Even minor injuries can result in bruising, swelling, and tenderness that may persist for several days.
1.7. Orchitis
Orchitis is an inflammation of the testicle, often caused by a viral or bacterial infection. It can occur as a result of mumps, a common childhood illness, or bacterial infections like epididymitis. Symptoms include testicular pain, swelling, fever, nausea, and fatigue.
1.8. Spermatocele
A spermatocele is a cyst that develops in the epididymis, typically containing fluid and dead sperm. These cysts are usually painless and small, but they can sometimes cause discomfort or a feeling of fullness in the scrotum if they grow larger.
1.9. Referred Pain
In some cases, testicular pain may be referred from another area of the body, such as the groin, abdomen, or back. Conditions like kidney stones, hernias, or nerve compression can sometimes cause pain that radiates to the testicles.
Understanding these potential causes is crucial for seeking appropriate medical attention and receiving an accurate diagnosis. If you are experiencing persistent or severe testicular pain, consult a healthcare professional promptly.
2. Understanding Varicocele
Varicocele is a common condition that affects the veins within the scrotum, similar to varicose veins in the legs. It occurs when the valves inside these veins fail to function properly, leading to blood pooling and enlargement of the veins. This condition can cause discomfort, pain, and, in some cases, fertility issues.
2.1. Anatomy of Varicocele
To understand varicocele, it’s essential to know the anatomy of the scrotum and its blood vessels. The testicles are suspended within the scrotum and receive blood supply from the testicular arteries. The veins responsible for draining blood from the testicles form a network called the pampiniform plexus, which eventually merges into the testicular veins.
:max_bytes(150000):strip_icc()/varicocele-overview-4588868-FINAL-1a9869c52a814367b362a2e54c9d3b3e.png)
2.2. How Varicocele Develops
Varicocele develops when the valves within the testicular veins become incompetent, preventing blood from flowing efficiently back to the heart. This leads to a backflow of blood, causing the veins to dilate and enlarge. Over time, these enlarged veins can become twisted and tangled, forming a varicocele.
2.3. Why Left Testicle Pain Is More Common
Varicoceles are more frequently observed on the left side due to anatomical differences in the venous drainage system. The left testicular vein drains into the left renal vein at a 90-degree angle, which can create increased pressure and resistance to blood flow. In contrast, the right testicular vein drains directly into the inferior vena cava, providing a more direct and less restrictive pathway.
2.4. Symptoms of Varicocele
The symptoms of varicocele can vary from person to person. Some individuals may experience no symptoms at all, while others may have significant discomfort. Common symptoms include:
- Dull or aching pain: A persistent, dull ache or throbbing sensation in the scrotum, which may worsen with standing, exercise, or prolonged sitting.
- Heaviness or dragging sensation: A feeling of heaviness or dragging in the scrotum, especially after physical activity.
- Enlarged veins: Visible or palpable enlarged veins in the scrotum, often described as feeling like a “bag of worms.”
- Testicular atrophy: In some cases, varicocele can lead to shrinkage or atrophy of the affected testicle.
- Infertility: Varicocele has been linked to infertility due to its potential impact on sperm production and quality.
2.5. Diagnosis of Varicocele
Varicocele is typically diagnosed through a physical examination by a healthcare provider. The doctor may palpate the scrotum to feel for enlarged veins. In some cases, an ultrasound of the scrotum may be ordered to confirm the diagnosis and rule out other potential causes of testicular pain.
2.6. Grading of Varicocele
Varicoceles are often graded based on their size and visibility during a physical examination:
- Grade 1: Small varicocele that can be felt only during the Valsalva maneuver (bearing down).
- Grade 2: Moderate varicocele that can be felt while standing.
- Grade 3: Large varicocele that is visible through the skin of the scrotum.
Understanding varicocele and its potential symptoms is crucial for seeking appropriate medical attention and exploring treatment options.
3. Treatment Options for Varicocele
There are several treatment options available for varicocele, ranging from conservative management to surgical interventions. The choice of treatment depends on various factors, including the severity of symptoms, the impact on fertility, and individual preferences.
3.1. Conservative Management
For individuals with mild symptoms or those who are not planning to have children, conservative management may be an appropriate approach. This involves measures to alleviate discomfort and manage symptoms without undergoing invasive procedures. Conservative strategies may include:
- Pain relievers: Over-the-counter pain medications such as ibuprofen or acetaminophen can help alleviate mild to moderate pain.
- Supportive underwear: Wearing supportive underwear or a jockstrap can provide scrotal support and reduce discomfort.
- Lifestyle modifications: Avoiding prolonged standing, heavy lifting, and activities that exacerbate symptoms may help improve comfort.
- Cold packs: Applying cold packs to the scrotum can help reduce swelling and relieve pain.
3.2. Surgical Interventions
When conservative measures are insufficient or when varicocele is causing significant pain or infertility, surgical intervention may be recommended. Several surgical options are available, including:
- Open surgery: This involves making an incision in the groin or abdomen to access and ligate (tie off) the affected veins. Open surgery can be performed using traditional surgical techniques or with the aid of a microscope (microsurgical varicocelectomy).
- Laparoscopic surgery: This minimally invasive approach involves making small incisions in the abdomen and using a laparoscope (a thin, flexible tube with a camera) to visualize and ligate the veins.
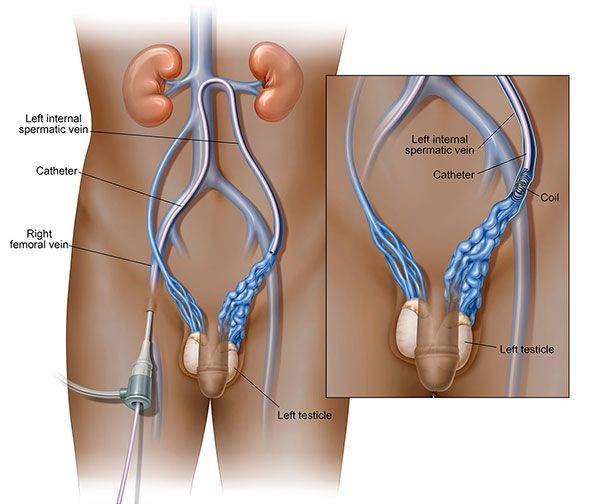
- Percutaneous embolization: This non-surgical procedure involves inserting a catheter into a vein in the groin or neck and guiding it to the affected veins in the scrotum. Once in position, coils or sclerosing agents are used to block the veins and redirect blood flow.
3.3. Varicocele Embolization: A Minimally Invasive Option
Varicocele embolization offers a minimally invasive alternative to traditional surgery for treating varicocele. This procedure is performed by an interventional radiologist and involves blocking the affected veins using coils or sclerosing agents.
3.3.1. How Varicocele Embolization Works
During varicocele embolization, a small catheter is inserted, usually through the groin or neck, and guided to the affected veins in the scrotum under real-time imaging guidance. Once the catheter is in position, coils or sclerosing agents are deployed to block the veins and redirect blood flow to healthy vessels.
3.3.2. Benefits of Varicocele Embolization
Varicocele embolization offers several advantages over traditional surgery, including:
- Minimally invasive: The procedure requires only a small puncture site, resulting in less pain, scarring, and recovery time compared to open surgery.
- Outpatient procedure: Varicocele embolization is typically performed on an outpatient basis, allowing patients to return home the same day.
- Shorter recovery time: Recovery from varicocele embolization is generally faster than with surgery, with most patients able to resume normal activities within a few days.
- High success rate: Varicocele embolization has a high success rate in relieving pain and improving fertility.
- Bilateral treatment: Embolization can be used to treat varicoceles on both sides of the scrotum during the same procedure.
3.3.3. Risks and Considerations
While varicocele embolization is generally safe and effective, it is essential to be aware of potential risks and considerations:
- Allergic reaction: Some patients may experience an allergic reaction to the contrast dye used during the procedure.
- Infection: As with any invasive procedure, there is a risk of infection at the puncture site.
- Coil migration: In rare cases, the coils used to block the veins may migrate to other areas of the body.
- Recurrence: Varicocele can recur after embolization, although this is relatively uncommon.
3.4. Comparing Treatment Options
The choice of treatment for varicocele depends on various factors, including the severity of symptoms, the impact on fertility, and individual preferences. Here’s a comparison of the different treatment options:
| Treatment Option | Description | Advantages | Disadvantages |
|---|---|---|---|
| Conservative Management | Pain relievers, supportive underwear, lifestyle modifications, cold packs. | Non-invasive, can provide relief for mild symptoms. | Does not address the underlying cause of varicocele, may not be effective for severe symptoms. |
| Open Surgery | Incision in the groin or abdomen to ligate the affected veins. | Effective for severe varicoceles, can be performed with microsurgical techniques to minimize complications. | More invasive than other options, longer recovery time, higher risk of complications such as infection and hydrocele formation. |
| Laparoscopic Surgery | Minimally invasive approach using small incisions and a laparoscope to visualize and ligate the veins. | Less invasive than open surgery, shorter recovery time, lower risk of complications. | Requires general anesthesia, may not be suitable for all patients. |
| Percutaneous Embolization | Catheter inserted into a vein to block the affected veins using coils or sclerosing agents. | Minimally invasive, outpatient procedure, shorter recovery time, high success rate, can treat bilateral varicoceles during the same procedure. | Risk of allergic reaction to contrast dye, infection at the puncture site, coil migration, recurrence. |
3.5. Considerations for Fertility
If varicocele is affecting fertility, treatment options may include surgery or embolization. Studies have shown that treating varicocele can improve sperm parameters and increase the chances of natural conception or success with assisted reproductive technologies such as in vitro fertilization (IVF).
Choosing the right treatment option for varicocele requires careful consideration and consultation with a healthcare provider. Factors to consider include the severity of symptoms, the impact on fertility, and individual preferences.
4. Testicular Torsion: A Medical Emergency
Testicular torsion is a serious condition that requires immediate medical attention. It occurs when the testicle rotates, twisting the spermatic cord and cutting off blood supply. This can lead to irreversible damage to the testicle if not treated promptly.
4.1. Understanding Testicular Torsion
The spermatic cord contains blood vessels, nerves, and the vas deferens, which carries sperm from the testicle. When the testicle rotates, it twists the spermatic cord, compressing the blood vessels and restricting blood flow to the testicle.
4.2. Symptoms of Testicular Torsion
The hallmark symptom of testicular torsion is sudden, severe testicular pain. Other symptoms may include:
- Sudden, intense pain: Severe pain in the testicle that comes on abruptly.
- Swelling: Swelling and tenderness in the scrotum.
- Nausea and vomiting: Nausea and vomiting may accompany the pain.
- Abdominal pain: Some individuals may experience pain in the lower abdomen.
- Elevated testicle: The affected testicle may be positioned higher than normal or at an unusual angle.
4.3. Risk Factors for Testicular Torsion
Testicular torsion can occur at any age but is most common in adolescents and young adults. Risk factors may include:
- Age: Adolescents and young adults are at higher risk.
- Bell clapper deformity: This anatomical abnormality occurs when the testicle is not properly anchored within the scrotum, allowing it to rotate more freely.
- Previous torsion: Individuals who have experienced testicular torsion in the past are at higher risk of recurrence.
- Family history: A family history of testicular torsion may increase the risk.
4.4. Diagnosis of Testicular Torsion
Testicular torsion is diagnosed based on a physical examination and imaging studies. A healthcare provider will assess the symptoms, examine the scrotum, and may order a Doppler ultrasound to evaluate blood flow to the testicle.
4.5. Treatment of Testicular Torsion
Testicular torsion requires immediate medical attention to restore blood flow to the testicle. The primary treatment is surgery to untwist the spermatic cord and secure the testicle in place to prevent future torsion.
4.5.1. Manual Detorsion
In some cases, a healthcare provider may attempt manual detorsion, which involves physically untwisting the spermatic cord by manipulating the testicle through the scrotum. However, even if manual detorsion is successful, surgery is still necessary to secure the testicle and prevent recurrence.
4.5.2. Surgical Exploration and Fixation
Surgical exploration involves making an incision in the scrotum to access the testicle and spermatic cord. The surgeon will untwist the spermatic cord and assess the viability of the testicle. If the testicle is still viable, it will be secured in place using sutures to prevent future torsion (orchiopexy). If the testicle is not viable due to prolonged lack of blood flow, it may need to be removed (orchiectomy).
4.6. Importance of Timely Intervention
The window of opportunity to save a testicle affected by torsion is limited. After about six hours of torsion, the risk of irreversible damage increases significantly. Therefore, it is crucial to seek medical attention immediately if you experience sudden, severe testicular pain.
Testicular torsion is a medical emergency that requires prompt diagnosis and treatment to prevent permanent damage to the testicle. If you experience sudden, severe testicular pain, seek medical attention immediately.
5. Other Potential Causes of Testicular Pain
While varicocele and testicular torsion are common causes of testicular pain, there are several other potential culprits to consider. Understanding these alternative causes can help in seeking appropriate medical attention and receiving an accurate diagnosis.
5.1. Epididymitis
Epididymitis is an inflammation of the epididymis, a coiled tube located at the back of the testicle that stores and carries sperm. This condition is often caused by a bacterial infection, including sexually transmitted infections (STIs) like chlamydia and gonorrhea.
5.1.1. Symptoms of Epididymitis
Symptoms of epididymitis may include:
- Testicular pain: Gradual onset of pain in the testicle, which may worsen over time.
- Swelling: Swelling and tenderness in the scrotum.
- Redness and warmth: Redness and warmth in the scrotum.
- Discharge: Discharge from the urethra.
- Painful urination: Pain or burning sensation during urination.
5.1.2. Treatment of Epididymitis
Treatment for epididymitis typically involves antibiotics to clear the infection. Pain relievers, scrotal support, and rest may also be recommended to alleviate symptoms.
5.2. Orchitis
Orchitis is an inflammation of the testicle, often caused by a viral or bacterial infection. It can occur as a result of mumps, a common childhood illness, or bacterial infections like epididymitis.
5.2.1. Symptoms of Orchitis
Symptoms of orchitis may include:
- Testicular pain: Pain in the testicle, which may be severe.
- Swelling: Swelling and tenderness in the scrotum.
- Fever: Fever may accompany the pain and swelling.
- Nausea and vomiting: Nausea and vomiting may occur.
5.2.2. Treatment of Orchitis
Treatment for orchitis depends on the underlying cause. Viral orchitis is typically treated with supportive care, such as pain relievers, rest, and scrotal support. Bacterial orchitis requires antibiotics to clear the infection.
5.3. Hydrocele
A hydrocele is a fluid-filled sac that surrounds a testicle, causing swelling in the scrotum. Hydroceles are usually painless, but they can cause discomfort or a feeling of heaviness in the scrotum, especially as they increase in size.
5.3.1. Symptoms of Hydrocele
Symptoms of hydrocele may include:
- Swelling: Swelling in the scrotum, which may be gradual or sudden.
- Discomfort: Discomfort or a feeling of heaviness in the scrotum.
- Pain: Pain is usually minimal, but large hydroceles can cause discomfort.
5.3.2. Treatment of Hydrocele
Hydroceles that are small and asymptomatic may not require treatment. Larger or symptomatic hydroceles can be treated with needle aspiration (draining the fluid with a needle) or surgery to remove the sac.
5.4. Spermatocele
A spermatocele is a cyst that develops in the epididymis, typically containing fluid and dead sperm. These cysts are usually painless and small, but they can sometimes cause discomfort or a feeling of fullness in the scrotum if they grow larger.
5.4.1. Symptoms of Spermatocele
Symptoms of spermatocele may include:
- Lump: A small, painless lump in the scrotum.
- Discomfort: Discomfort or a feeling of fullness in the scrotum.
5.4.2. Treatment of Spermatocele
Spermatoceles that are small and asymptomatic may not require treatment. Larger or symptomatic spermatoceles can be treated with surgery to remove the cyst.
5.5. Testicular Cancer
Testicular cancer is a relatively rare cancer that affects the testicles. Although less common, it is important to consider testicular cancer as a potential cause of testicular pain or discomfort.
5.5.1. Symptoms of Testicular Cancer
Symptoms of testicular cancer may include:
- Lump: A lump in the testicle, which may be painless or tender.
- Swelling: Swelling or enlargement of the testicle.
- Heaviness: A feeling of heaviness in the scrotum.
- Pain: Pain or discomfort in the testicle or scrotum.
5.5.2. Diagnosis and Treatment of Testicular Cancer
If you notice any of these symptoms, it is important to see a doctor immediately. Early detection and treatment of testicular cancer can result in a complete cure.
5.6. Inguinal Hernia
An inguinal hernia occurs when tissue, such as part of the intestine, protrudes through a weak spot in the abdominal muscles. This can sometimes cause pain or discomfort in the groin or scrotum.
5.6.1. Symptoms of Inguinal Hernia
Symptoms of inguinal hernia may include:
- Bulge: A visible bulge in the groin or scrotum.
- Pain: Pain or discomfort in the groin or scrotum, especially when coughing, straining, or lifting heavy objects.
- Heaviness: A feeling of heaviness or pressure in the groin.
5.6.2. Treatment of Inguinal Hernia
Treatment for inguinal hernia typically involves surgery to repair the weakened abdominal muscles and prevent the tissue from protruding.
5.7. Kidney Stones
Kidney stones are hard deposits that form in the kidneys and can cause severe pain as they pass through the urinary tract. In some cases, kidney stones can cause referred pain to the groin or testicles.
5.7.1. Symptoms of Kidney Stones
Symptoms of kidney stones may include:
- Severe pain: Severe pain in the side, back, or lower abdomen.
- Painful urination: Pain or burning sensation during urination.
- Blood in urine: Blood in the urine (hematuria).
- Nausea and vomiting: Nausea and vomiting may occur.
5.7.2. Treatment of Kidney Stones
Treatment for kidney stones depends on the size and location of the stones. Small stones may pass on their own with increased fluid intake and pain relievers. Larger stones may require medical intervention, such as shock wave lithotripsy (SWL) or surgery.
5.8. Nerve Pain
Nerve pain in the groin or scrotum can be caused by nerve compression, injury, or inflammation. This can result in chronic testicular pain or discomfort.
5.8.1. Symptoms of Nerve Pain
Symptoms of nerve pain may include:
- Burning pain: Burning or shooting pain in the groin or scrotum.
- Numbness or tingling: Numbness or tingling sensation in the groin or scrotum.
- Sensitivity: Increased sensitivity to touch in the affected area.
5.8.2. Treatment of Nerve Pain
Treatment for nerve pain depends on the underlying cause and may include pain relievers, nerve blocks, physical therapy, or surgery.
6. When to Seek Medical Attention
While some causes of testicular pain may be minor and self-limiting, it is important to know when to seek medical attention. Prompt medical evaluation is necessary for certain symptoms or situations to rule out serious conditions and prevent potential complications.
6.1. Sudden, Severe Pain
If you experience sudden, severe testicular pain, especially if accompanied by swelling, nausea, or vomiting, seek medical attention immediately. This could be a sign of testicular torsion, a medical emergency that requires prompt treatment to prevent permanent damage to the testicle.
6.2. Persistent Pain
If you have persistent testicular pain that lasts for more than a few days, even if it is mild, it is important to see a doctor. Chronic testicular pain can be a sign of an underlying condition that requires medical evaluation and treatment.
6.3. Lump or Swelling
If you notice a lump or swelling in your testicle, see a doctor promptly. This could be a sign of testicular cancer or another serious condition that requires medical attention.
6.4. Fever or Infection
If you have testicular pain accompanied by fever, chills, redness, or warmth in the scrotum, this could be a sign of an infection that requires antibiotics.
6.5. Trauma or Injury
If you have experienced trauma or injury to the testicles, it is important to see a doctor to rule out serious damage and receive appropriate treatment.
6.6. Difficulty Urinating
If you have testicular pain accompanied by difficulty urinating, frequent urination, or blood in the urine, see a doctor to evaluate for potential urinary tract infections or kidney stones.
6.7. Fertility Concerns
If you are experiencing testicular pain and are concerned about its potential impact on your fertility, see a doctor to discuss evaluation and treatment options.
7. Diagnostic Tests for Testicular Pain
When evaluating testicular pain, healthcare providers may use various diagnostic tests to determine the underlying cause. These tests can help rule out serious conditions and guide treatment decisions.
7.1. Physical Examination
The first step in evaluating testicular pain is a thorough physical examination. The healthcare provider will examine the scrotum, palpate the testicles, and assess for any signs of swelling, tenderness, or abnormalities.
7.2. Ultrasound
An ultrasound is a non-invasive imaging test that uses sound waves to create images of the testicles and surrounding structures. It can help identify abnormalities such as varicoceles, hydroceles, spermatoceles, tumors, or signs of infection.
7.3. Doppler Ultrasound
A Doppler ultrasound is a type of ultrasound that measures blood flow to the testicles. It can help diagnose testicular torsion by detecting reduced or absent blood flow to the affected testicle.
7.4. Urine Analysis
A urine analysis involves examining a sample of urine to check for signs of infection, blood, or other abnormalities. It can help diagnose urinary tract infections or kidney stones.
7.5. Blood Tests
Blood tests may be ordered to check for signs of infection, inflammation, or testicular cancer. Tumor markers, such as alpha-fetoprotein (AFP) and human chorionic gonadotropin (hCG), may be elevated in cases of testicular cancer.
7.6. Scrotal Exploration
In some cases, a scrotal exploration (surgical exploration of the scrotum) may be necessary to diagnose and treat testicular pain. This involves making an incision in the scrotum to visualize the testicles and surrounding structures.
8. Prevention Strategies for Testicular Pain
While not all causes of testicular pain can be prevented, there are certain measures you can take to reduce your risk and maintain testicular health.
8.1. Practice Safe Sex
Practicing safe sex, including using condoms, can help prevent sexually transmitted infections (STIs) that can cause epididymitis or orchitis.
8.2. Get Vaccinated
Getting vaccinated against mumps can help prevent mumps orchitis, a viral infection that can cause inflammation of the testicles.
8.3. Wear Protective Gear
Wearing protective gear, such as a jockstrap, during sports or other activities that involve a risk of testicular injury can help prevent trauma to the testicles.
8.4. Perform Self-Exams
Performing regular testicular self-exams can help you detect any lumps, swelling, or abnormalities early on. This can improve the chances of early diagnosis and treatment for testicular cancer or other conditions.
8.5. Maintain a Healthy Lifestyle
Maintaining a healthy lifestyle, including eating a balanced diet, exercising regularly, and avoiding smoking and excessive alcohol consumption, can promote overall health and reduce the risk of certain conditions that can cause testicular pain.
8.6. Avoid Prolonged Sitting or Standing
Avoiding prolonged sitting or standing, especially in hot environments, can help reduce the risk of varicocele formation.
9. Home Remedies for Testicular Pain Relief
While it is important to seek medical attention for persistent or severe testicular pain, there are some home remedies that may help relieve mild discomfort.
9.1. Rest
Resting and avoiding strenuous activities can help reduce pain and inflammation in the testicles.
9.2. Ice Packs
Applying ice packs to the scrotum for 15-20 minutes at a time can help reduce swelling and relieve pain.
9.3. Warm Baths
Taking warm baths can help relax the muscles in the scrotum and relieve pain.
9.4. Scrotal Support
Wearing supportive underwear or a jockstrap can provide scrotal support and reduce discomfort.
9.5. Over-the-Counter Pain Relievers
Over-the-counter pain relievers such as ibuprofen or acetaminophen can help alleviate mild to moderate pain.
10. Addressing the Psychological Impact of Testicular Pain
Testicular pain can have a significant psychological impact on individuals, affecting their mood, self-esteem, and quality of life. It is important to address these psychological aspects of testicular pain and seek support when needed.
10.1. Understanding the Emotional Toll
Chronic testicular pain can lead to feelings of frustration, anxiety, depression, and isolation. It can also impact sexual function and relationships.
10.2. Seeking Psychological Support
If you are struggling with the psychological impact of testicular pain, consider seeking support from a mental health professional. A therapist or counselor can help you cope with your emotions, develop strategies for managing stress, and improve your overall well-being.
10.3. Joining Support Groups
Joining a support group can provide a sense of community and connection with others who understand what you are going through. Sharing your experiences and learning from others can be helpful in coping with testicular pain.
10.4. Practicing Self-Care
Practicing self-care activities, such as exercise, meditation, or hobbies, can help improve your mood and reduce stress.
Testicular pain can be a distressing symptom with a variety of potential causes. Understanding the possible causes, seeking appropriate medical attention, and implementing prevention strategies can help maintain testicular health and improve your overall well-being. At WHY.EDU.VN, we understand the challenges you face in finding reliable answers, which is why we are committed to providing you with accurate and accessible information.
Experiencing testicular pain can be worrying, and finding the right answers quickly is essential. WHY.EDU.VN is here to help you navigate your questions and concerns. Do you have more questions or need personalized advice? Contact us at 101 Curiosity Lane, Answer Town, CA 90210, United States, or reach out via WhatsApp at +1 (213) 555-0101. Visit our website at why.edu.vn to ask a question and connect with experts who can provide the answers you need. Let us help you find peace of mind and the right path forward.
Frequently Asked Questions (FAQ)
1. Is testicular pain always a sign of something serious?
Not always, but it’s crucial to get it checked by a doctor to rule out serious conditions like testicular torsion or cancer.
2. Can wearing tight underwear cause testicular pain?
Yes, tight underwear can sometimes cause discomfort or pain by compressing the testicles.
3. How can I tell if my testicular pain is an emergency?
If you experience sudden, severe pain, especially with swelling, nausea, or vomiting, seek immediate medical attention.
4. Can exercise cause testicular pain?
Yes, strenuous exercise can sometimes cause testicular pain, especially if you’re not wearing proper support.
5. What is the difference between epididymitis and orchitis?
Epididymitis is inflammation of the epididymis, while orchitis is inflammation of the testicle itself.
6. Can stress cause testicular pain?
While stress itself may not directly cause testicular pain, it can exacerbate existing conditions.
7. What are the long-term effects of varicocele?
Varicocele can lead to infertility and low testosterone levels if left untreated.
8. How often should I perform a testicular self-exam?
You should perform a testicular self-exam monthly to check for any abnormalities.
9. Can testicular pain affect my sex life?
Yes, testicular pain can affect your sex drive and ability to have intercourse.
10. Are there any alternative treatments for testicular pain?
Some people find relief with alternative therapies like acupuncture or herbal remedies, but always consult with a doctor first.