Why Does Anal Hurt? Anal discomfort can stem from various underlying causes, ranging from common issues like hemorrhoids and fissures to less frequent conditions such as infections or pelvic floor dysfunction. WHY.EDU.VN provides a comprehensive resource to explore these potential reasons and offer effective solutions for relief and prevention. Understanding the underlying causes can help you find the right treatment for anal pain, rectal pain and pelvic pain.
1. Common Causes of Anal Pain: An Overview
Anal pain can be a distressing symptom with numerous potential causes. It is important to get the proper diagnosis to seek treatment. Let’s take a look at some of the most common reasons behind anal discomfort.
1.1 Hemorrhoids
Hemorrhoids are swollen veins in the anus and rectum that can cause pain, itching, and bleeding.
- What are Hemorrhoids?: These are vascular structures in the anal canal, acting as cushions to aid in bowel control.
- Causes: Straining during bowel movements, chronic constipation or diarrhea, pregnancy, and obesity can all increase pressure on these veins, leading to hemorrhoids.
- Symptoms: Painless bleeding during bowel movements, itching or irritation in the anal area, discomfort while sitting, and swelling around the anus are common indicators.
- Diagnosis: A physical exam can often identify external hemorrhoids, while internal hemorrhoids may require a digital rectal exam or anoscopy.
- Treatment: Mild cases often respond to lifestyle changes like increasing fiber and water intake. Over-the-counter creams and suppositories can provide temporary relief. More severe cases may require procedures like rubber band ligation or surgery. According to the University of California San Francisco, “Most hemorrhoids can be treated with home remedies. Only a small percentage of people need medical treatment.”
- Prevention: Preventative measures include maintaining a high-fiber diet, staying hydrated, avoiding straining during bowel movements, and practicing good hygiene.
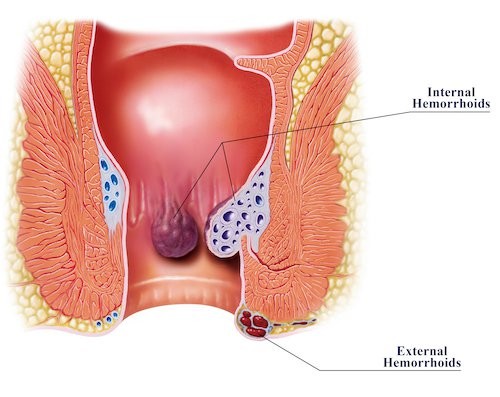 Medical diagram illustrating internal and external hemorrhoids in the anal canal
Medical diagram illustrating internal and external hemorrhoids in the anal canal
1.2 Anal Fissures
Anal fissures are small tears in the lining of the anus, often caused by passing hard stools.
- What are Anal Fissures?: These are cuts or tears in the delicate skin lining the anal canal.
- Causes: Common causes include constipation, straining during bowel movements, chronic diarrhea, and anal sex.
- Symptoms: Sharp pain during bowel movements, followed by a throbbing ache, and blood on the stool or toilet paper are typical symptoms.
- Diagnosis: A visual examination of the anus is usually sufficient for diagnosis.
- Treatment: Treatment focuses on relieving pain and promoting healing. This may include stool softeners, topical anesthetics, and sitz baths. In some cases, Botox injections or surgery may be necessary. The Cleveland Clinic notes that “Most anal fissures heal on their own with conservative treatment.”
- Prevention: Preventing constipation and straining is key to preventing anal fissures. This can be achieved through a high-fiber diet, adequate hydration, and regular exercise.
1.3 Anal Abscesses and Fistulas
These conditions involve infections and abnormal connections in the anal region.
- What are Anal Abscesses and Fistulas?: An abscess is a collection of pus caused by an infection, while a fistula is an abnormal tunnel connecting the abscess to the skin near the anus.
- Causes: Abscesses typically result from infected anal glands. Fistulas often develop after an abscess has been drained.
- Symptoms: Symptoms of an abscess include persistent throbbing pain, swelling, redness, and fever. Fistulas can cause pain, drainage of pus, and irritation around the anus.
- Diagnosis: A physical exam can usually identify an abscess. Fistulas may require imaging tests like MRI or CT scans.
- Treatment: Abscesses require drainage, usually through a surgical incision. Fistulas often require surgery to close the abnormal tunnel. Antibiotics may also be prescribed. According to the American Society of Colon and Rectal Surgeons, “Most anal fistulas require surgical treatment to be cured.”
- Prevention: Maintaining good hygiene and addressing underlying conditions like Crohn’s disease can help prevent these issues.
1.4 Proctalgia Fugax
This condition causes sudden, severe rectal pain due to muscle spasms.
- What is Proctalgia Fugax?: This is a benign condition characterized by fleeting episodes of intense rectal pain caused by spasms of the levator ani muscle.
- Causes: The exact cause is unknown, but factors like stress, anxiety, and certain bowel habits may play a role.
- Symptoms: Sudden, sharp, or cramping pain in the rectum that lasts for a few seconds to minutes. Episodes are unpredictable and can occur at any time.
- Diagnosis: Diagnosis is based on symptoms and a physical exam to rule out other conditions.
- Treatment: There is no specific treatment for proctalgia fugax. Pain relief measures like warm baths, massage, and relaxation techniques may help. In some cases, muscle relaxants may be prescribed.
- Prevention: Since the cause is unknown, there are no specific preventative measures. Managing stress and practicing relaxation techniques may reduce the frequency of episodes.
1.5 Levator Ani Syndrome
This chronic condition involves pain and pressure in the rectum and pelvic area due to muscle tension.
- What is Levator Ani Syndrome?: This is a chronic pain condition caused by spasm or tension in the levator ani muscle, which supports the pelvic floor.
- Causes: The exact cause is unknown, but factors like stress, poor posture, and pelvic floor dysfunction may contribute.
- Symptoms: Aching, pressure, or pain in the rectum, perineum, or lower back. Pain may worsen with sitting or bowel movements.
- Diagnosis: Diagnosis involves a physical exam and assessment of symptoms.
- Treatment: Treatment options include physical therapy, biofeedback, massage, and pain medication.
- Prevention: Maintaining good posture, practicing relaxation techniques, and addressing pelvic floor dysfunction may help prevent this condition.
1.6 Pruritus Ani
This is a condition characterized by intense itching around the anus.
- What is Pruritus Ani?: This is a common condition characterized by intense itching around the anus.
- Causes: Causes can include poor hygiene, excessive cleaning, irritants like soaps and detergents, infections, and skin conditions like eczema.
- Symptoms: Intense itching, burning, and soreness around the anus.
- Diagnosis: Diagnosis is based on a physical exam and review of symptoms.
- Treatment: Treatment involves identifying and eliminating the cause of the itching. This may include improving hygiene, avoiding irritants, and using topical creams or ointments.
- Prevention: Practicing good hygiene, avoiding irritants, and keeping the anal area dry can help prevent pruritus ani.
1.7 Sexually Transmitted Infections (STIs)
STIs like herpes, gonorrhea, and chlamydia can cause anal pain and discomfort.
- How STIs Affect the Anus: STIs can cause inflammation, sores, and pain in the anal area.
- Common STIs Causing Anal Pain:
- Herpes: Causes painful blisters and sores.
- Gonorrhea and Chlamydia: Can cause rectal pain, discharge, and itching.
- Syphilis: Can cause a chancre (sore) in the anal area.
- Symptoms: Anal pain, itching, discharge, sores, and bleeding are common symptoms.
- Diagnosis: Diagnosis involves a physical exam and laboratory tests to identify the specific STI.
- Treatment: Treatment depends on the specific STI and may include antibiotics, antiviral medications, or topical creams.
- Prevention: Practicing safe sex, including using condoms, is the best way to prevent STIs. Regular STI testing is also important, especially for individuals with multiple partners. The Centers for Disease Control and Prevention (CDC) recommends that all sexually active individuals get tested for STIs regularly.
1.8 Other Infections
Other infections, such as fungal infections, can also lead to anal pain.
- Fungal Infections: Yeast infections can occur in the anal area, causing itching, redness, and discomfort.
- Bacterial Infections: Bacterial infections can also cause anal pain and inflammation.
- Symptoms: Symptoms may include itching, burning, pain, redness, and discharge.
- Diagnosis: Diagnosis involves a physical exam and laboratory tests to identify the specific infection.
- Treatment: Treatment depends on the type of infection and may include antifungal creams, antibiotics, or other medications.
- Prevention: Practicing good hygiene, keeping the anal area clean and dry, and avoiding irritants can help prevent infections.
1.9 Anal Cancer
Although rare, anal cancer can cause pain and bleeding.
- What is Anal Cancer?: This is a rare type of cancer that develops in the anus.
- Causes: Risk factors include HPV infection, smoking, and a weakened immune system.
- Symptoms: Anal pain, bleeding, itching, a lump near the anus, and changes in bowel habits are potential symptoms.
- Diagnosis: Diagnosis involves a physical exam, anoscopy, and biopsy.
- Treatment: Treatment may include surgery, radiation therapy, and chemotherapy.
- Prevention: HPV vaccination and avoiding smoking can help reduce the risk of anal cancer. Regular check-ups and screenings are also important, especially for individuals at high risk. The American Cancer Society provides detailed information on anal cancer prevention and screening.
2. When to Seek Medical Attention for Anal Pain
It’s crucial to know when anal pain warrants a visit to a healthcare professional.
2.1 Persistent or Severe Pain
If your anal pain is persistent, severe, or worsening, seek medical attention.
- Why It’s Important: Persistent or severe pain could indicate a serious underlying condition that requires prompt treatment.
- What to Do: Schedule an appointment with your doctor or a specialist for a thorough evaluation.
2.2 Bleeding
Any bleeding from the anus should be evaluated by a doctor.
- Why It’s Important: Bleeding can be a symptom of various conditions, including hemorrhoids, fissures, infections, and even cancer.
- What to Do: Consult your doctor to determine the cause of the bleeding and receive appropriate treatment.
2.3 Changes in Bowel Habits
Changes in bowel habits, such as constipation, diarrhea, or changes in stool consistency, should be discussed with a healthcare provider.
- Why It’s Important: These changes can be signs of underlying digestive issues or other medical conditions.
- What to Do: Keep track of your bowel habits and discuss any significant changes with your doctor.
2.4 Fever or Other Systemic Symptoms
If you experience fever, chills, or other systemic symptoms along with anal pain, seek immediate medical attention.
- Why It’s Important: These symptoms could indicate a serious infection or other medical emergency.
- What to Do: Go to the nearest emergency room or urgent care center for evaluation and treatment.
2.5 Failure to Improve with Self-Care
If your anal pain does not improve with self-care measures like over-the-counter treatments and lifestyle changes, it’s time to see a doctor.
- Why It’s Important: Failure to improve with self-care could mean that your condition requires more specialized treatment.
- What to Do: Schedule an appointment with your doctor for further evaluation and management.
3. Diagnostic Procedures for Anal Pain
Doctors use various methods to diagnose the cause of anal pain.
3.1 Physical Examination
A physical exam is often the first step in diagnosing anal pain.
- What to Expect: The doctor will visually inspect the anal area for signs of hemorrhoids, fissures, or other abnormalities. They may also perform a digital rectal exam to feel for any masses or irregularities.
3.2 Anoscopy
An anoscopy involves using a small scope to examine the anal canal.
- What It Is: An anoscope is a short, rigid tube with a light that allows the doctor to visualize the lining of the anal canal.
- Purpose: Anoscopy can help identify internal hemorrhoids, fissures, and other conditions that may not be visible during a physical exam.
3.3 Sigmoidoscopy
A sigmoidoscopy is a procedure to examine the lower part of the colon.
- What It Is: A sigmoidoscope is a flexible tube with a camera that is inserted into the rectum to visualize the lower colon.
- Purpose: Sigmoidoscopy can help identify inflammation, polyps, or other abnormalities in the colon that may be contributing to anal pain.
3.4 Colonoscopy
A colonoscopy allows the doctor to view the entire colon.
- What It Is: A colonoscope is a flexible tube with a camera that is inserted into the rectum to visualize the entire colon.
- Purpose: Colonoscopy is used to screen for colorectal cancer and other conditions that may be causing anal pain.
3.5 Imaging Tests
Imaging tests like MRI or CT scans may be used to evaluate more complex cases.
- What They Are: MRI and CT scans are non-invasive imaging techniques that can provide detailed images of the anal area and surrounding tissues.
- Purpose: These tests can help identify abscesses, fistulas, and other conditions that may not be visible during a physical exam or endoscopy.
4. Treatment Options for Anal Pain
There are several effective strategies to manage and alleviate anal pain.
4.1 Home Remedies
Many cases of anal pain can be managed with simple home remedies.
- Sitz Baths: Soaking in warm water for 10-15 minutes several times a day can relieve pain and inflammation.
- Topical Creams and Ointments: Over-the-counter creams containing hydrocortisone or lidocaine can provide temporary relief from itching and pain.
- Stool Softeners: These can help prevent constipation and straining, making bowel movements easier and less painful.
- Fiber Supplements: Increasing fiber intake can promote regular bowel movements and prevent constipation.
- Proper Hygiene: Gently cleaning the anal area with mild soap and water after each bowel movement can help prevent irritation.
4.2 Medications
Various medications can help alleviate anal pain and address underlying conditions.
- Pain Relievers: Over-the-counter pain relievers like acetaminophen or ibuprofen can help reduce pain and inflammation.
- Topical Corticosteroids: These can reduce inflammation and itching in the anal area.
- Muscle Relaxants: These may be prescribed to relieve muscle spasms in the pelvic floor.
- Antibiotics: Antibiotics are used to treat bacterial infections causing anal pain.
4.3 Medical Procedures
Some conditions may require medical procedures to resolve anal pain.
- Hemorrhoid Treatment: Procedures like rubber band ligation, sclerotherapy, or surgery may be used to treat severe hemorrhoids.
- Fissure Treatment: Botox injections or lateral internal sphincterotomy (LIS) may be used to relax the anal sphincter and promote healing of fissures.
- Abscess Drainage: Incision and drainage are necessary to treat anal abscesses.
- Fistula Surgery: Surgery is often required to close anal fistulas.
4.4 Physical Therapy
Physical therapy can be beneficial for conditions like levator ani syndrome.
- Pelvic Floor Therapy: This type of therapy can help strengthen and relax the pelvic floor muscles, reducing pain and improving function.
- Biofeedback: Biofeedback can help individuals learn to control their pelvic floor muscles and reduce pain.
5. Preventive Measures for Anal Pain
Adopting certain habits can help prevent anal pain and discomfort.
5.1 Maintain a Healthy Diet
A balanced diet rich in fiber can promote regular bowel movements and prevent constipation.
- High-Fiber Foods: Include plenty of fruits, vegetables, whole grains, and legumes in your diet.
- Limit Processed Foods: Reduce your intake of processed foods, which are often low in fiber and can contribute to constipation.
5.2 Stay Hydrated
Drinking plenty of water can help keep stools soft and prevent constipation.
- Recommended Intake: Aim for at least eight glasses of water per day.
5.3 Practice Good Hygiene
Keeping the anal area clean and dry can help prevent irritation and infection.
- Gentle Cleaning: Clean the anal area gently with mild soap and water after each bowel movement.
- Avoid Irritants: Avoid using harsh soaps, detergents, or perfumes in the anal area.
5.4 Avoid Straining During Bowel Movements
Straining during bowel movements can increase pressure on the anal veins and lead to hemorrhoids and fissures.
- Take Your Time: Allow yourself enough time to have a bowel movement without rushing or straining.
- Proper Posture: Elevating your feet with a small stool can help facilitate easier bowel movements.
5.5 Regular Exercise
Regular physical activity can promote healthy bowel function and prevent constipation.
- Recommended Activity: Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
5.6 Safe Sexual Practices
Practicing safe sex, including using condoms, can help prevent STIs that can cause anal pain.
- Condom Use: Use condoms consistently and correctly during anal sex.
- Regular STI Testing: Get tested for STIs regularly, especially if you have multiple partners.
6. Addressing Psychological Factors
Stress and anxiety can exacerbate anal pain.
6.1 Stress Management Techniques
Techniques like meditation, yoga, and deep breathing exercises can help reduce stress and anxiety.
- Mindfulness Meditation: Practicing mindfulness meditation can help you become more aware of your thoughts and feelings, reducing stress and anxiety.
- Yoga: Yoga combines physical postures, breathing exercises, and meditation to promote relaxation and reduce stress.
- Deep Breathing Exercises: Deep breathing exercises can help calm the nervous system and reduce anxiety.
6.2 Counseling or Therapy
Counseling or therapy can help individuals cope with chronic pain and address underlying psychological issues.
- Cognitive Behavioral Therapy (CBT): CBT can help individuals change negative thought patterns and behaviors that contribute to pain and distress.
- Support Groups: Joining a support group can provide a sense of community and support for individuals living with chronic pain.
7. Special Considerations for Women
Women may experience anal pain due to specific gynecological or obstetric conditions.
7.1 Pregnancy
Pregnancy can increase the risk of hemorrhoids and other conditions that cause anal pain.
- Hormonal Changes: Hormonal changes during pregnancy can relax the anal veins, making them more prone to swelling.
- Increased Pressure: The growing uterus can put pressure on the anal veins, increasing the risk of hemorrhoids.
- Constipation: Pregnancy can also cause constipation, which can contribute to anal pain.
- Management: Pregnant women can manage anal pain with home remedies like sitz baths, topical creams, and stool softeners. Consulting with a healthcare provider is important for proper management.
7.2 Endometriosis
Endometriosis can sometimes affect the rectum and cause anal pain.
- What is Endometriosis?: This is a condition in which the tissue that normally lines the uterus grows outside of it.
- How It Affects the Anus: Endometriosis can sometimes affect the rectum and cause pain, especially during bowel movements or menstruation.
- Diagnosis: Diagnosis may involve imaging tests like MRI or colonoscopy.
- Treatment: Treatment options include pain medication, hormone therapy, and surgery.
7.3 Childbirth
Childbirth can sometimes cause anal fissures or hemorrhoids.
- Straining During Delivery: Straining during childbirth can put pressure on the anal veins and cause hemorrhoids or fissures.
- Management: Postpartum anal pain can be managed with home remedies like sitz baths, topical creams, and stool softeners. Consulting with a healthcare provider is important for proper management.
8. Special Considerations for Men
Men may experience anal pain due to specific urological or prostate conditions.
8.1 Prostatitis
Prostatitis, an inflammation of the prostate gland, can cause referred pain to the anal area.
- What is Prostatitis?: This is an inflammation of the prostate gland.
- How It Affects the Anus: Prostatitis can cause pain in the pelvic area, including the rectum and anus.
- Symptoms: Symptoms may include pain, difficulty urinating, and frequent urination.
- Diagnosis: Diagnosis involves a physical exam, urine tests, and other tests to evaluate the prostate gland.
- Treatment: Treatment may include antibiotics, pain medication, and alpha-blockers to relax the muscles in the prostate and bladder.
8.2 Prostate Cancer
Although less common, prostate cancer can sometimes cause anal pain.
- What is Prostate Cancer?: This is a cancer that develops in the prostate gland.
- How It Affects the Anus: Prostate cancer can sometimes cause pain in the pelvic area, including the rectum and anus.
- Symptoms: Symptoms may include difficulty urinating, frequent urination, and pain in the back, hips, or pelvis.
- Diagnosis: Diagnosis involves a physical exam, prostate-specific antigen (PSA) test, and biopsy.
- Treatment: Treatment options include surgery, radiation therapy, hormone therapy, and chemotherapy.
9. The Role of Diet and Nutrition
A healthy diet plays a crucial role in preventing and managing anal pain.
9.1 Fiber-Rich Foods
Including plenty of fiber-rich foods in your diet can promote regular bowel movements and prevent constipation.
- Examples of Fiber-Rich Foods: Fruits, vegetables, whole grains, and legumes.
- Benefits of Fiber: Fiber adds bulk to the stool, making it easier to pass, and can also help regulate bowel movements.
9.2 Probiotics
Probiotics can help maintain a healthy balance of bacteria in the gut, which can improve digestion and prevent constipation.
- Sources of Probiotics: Yogurt, kefir, sauerkraut, and probiotic supplements.
- Benefits of Probiotics: Probiotics can help improve digestion, reduce inflammation, and boost the immune system.
9.3 Foods to Avoid
Certain foods can irritate the digestive system and worsen anal pain.
- Spicy Foods: Spicy foods can irritate the lining of the anus and cause discomfort.
- Caffeine and Alcohol: These substances can dehydrate the body and contribute to constipation.
- Processed Foods: Processed foods are often low in fiber and can contribute to constipation.
10. Alternative Therapies for Anal Pain
Some people find relief from anal pain through alternative therapies.
10.1 Acupuncture
Acupuncture involves inserting thin needles into specific points on the body to stimulate healing.
- How It Works: Acupuncture is believed to work by stimulating the release of endorphins, which are natural pain relievers.
- Benefits: Some people find that acupuncture helps relieve anal pain and discomfort.
10.2 Herbal Remedies
Certain herbal remedies may help alleviate anal pain and inflammation.
- Aloe Vera: Aloe vera has anti-inflammatory properties and can be applied topically to soothe irritated skin.
- Witch Hazel: Witch hazel can help reduce inflammation and itching in the anal area.
10.3 Biofeedback
Biofeedback can help individuals learn to control their pelvic floor muscles and reduce pain.
- How It Works: Biofeedback involves using sensors to monitor muscle activity and provide feedback to the individual, allowing them to learn how to control their muscles.
- Benefits: Biofeedback can help individuals with levator ani syndrome and other pelvic floor disorders reduce pain and improve function.
11. Latest Research and Developments
Ongoing research continues to improve our understanding and treatment of anal pain.
11.1 New Medications
Researchers are developing new medications to treat conditions like hemorrhoids and fissures.
11.2 Minimally Invasive Procedures
New minimally invasive procedures are being developed to treat anal pain with less pain and faster recovery times.
11.3 Advances in Pelvic Floor Therapy
Advances in pelvic floor therapy are improving the effectiveness of this treatment for conditions like levator ani syndrome.
12. Expert Opinions on Anal Pain
Experts emphasize the importance of seeking medical attention for persistent anal pain.
12.1 Importance of Early Diagnosis
Early diagnosis and treatment can help prevent complications and improve outcomes.
12.2 Personalized Treatment Plans
Treatment plans should be tailored to the individual’s specific condition and needs.
12.3 Multidisciplinary Approach
A multidisciplinary approach involving doctors, physical therapists, and other healthcare professionals can provide the best care for individuals with anal pain.
13. Case Studies and Success Stories
Real-life examples can provide hope and inspiration.
13.1 Case Study 1: Successful Management of Chronic Fissures
A patient with chronic anal fissures found relief through a combination of lifestyle changes, medication, and minimally invasive procedures.
13.2 Case Study 2: Overcoming Levator Ani Syndrome
A patient with levator ani syndrome improved their quality of life through physical therapy, biofeedback, and stress management techniques.
13.3 Case Study 3: Early Detection and Treatment of Anal Cancer
A patient who was diagnosed with anal cancer at an early stage was successfully treated with surgery and radiation therapy.
14. Debunking Myths About Anal Pain
Common misconceptions can prevent people from seeking proper care.
14.1 Myth: Anal Pain is Always Caused by Hemorrhoids
While hemorrhoids are a common cause of anal pain, there are many other potential causes.
14.2 Myth: Anal Pain is Nothing to Worry About
Persistent or severe anal pain should always be evaluated by a healthcare professional.
14.3 Myth: There is Nothing You Can Do About Anal Pain
There are many effective treatments for anal pain, and most people can find relief with proper care.
15. Living with Anal Pain: Tips for Coping
Practical advice for managing daily life with anal pain.
15.1 Comfortable Sitting Positions
Use cushions or pillows to make sitting more comfortable.
15.2 Loose-Fitting Clothing
Wear loose-fitting clothing to avoid irritating the anal area.
15.3 Emotional Support
Seek emotional support from friends, family, or a therapist.
16. Resources and Support for Anal Pain Sufferers
Organizations and websites that provide information and support.
16.1 Online Forums
Online forums can provide a sense of community and support for individuals with anal pain.
16.2 Support Groups
Support groups can provide a safe and supportive environment for sharing experiences and learning coping strategies.
16.3 Medical Websites
Reputable medical websites can provide accurate information about anal pain and its causes.
17. FAQ About Anal Pain
1. What are the most common causes of anal pain?
Hemorrhoids, anal fissures, and infections are among the most common causes.
2. When should I see a doctor for anal pain?
If the pain is severe, persistent, or accompanied by bleeding, seek medical attention.
3. Can diet affect anal pain?
Yes, a high-fiber diet can help prevent constipation and reduce anal pain.
4. What home remedies can help relieve anal pain?
Sitz baths, topical creams, and stool softeners can provide relief.
5. Is anal pain always a sign of a serious condition?
Not always, but it’s important to get it checked out to rule out serious causes.
6. Can STIs cause anal pain?
Yes, certain STIs can cause anal pain and discomfort.
7. What is levator ani syndrome?
It’s a chronic condition involving pain and pressure in the rectum and pelvic area due to muscle tension.
8. How is anal cancer diagnosed?
Diagnosis involves a physical exam, anoscopy, and biopsy.
9. Can stress and anxiety affect anal pain?
Yes, stress and anxiety can exacerbate anal pain.
10. What alternative therapies can help relieve anal pain?
Acupuncture, herbal remedies, and biofeedback may provide relief.Conclusion
Anal pain can be a challenging condition, but understanding its causes, seeking appropriate medical care, and adopting preventive measures can lead to effective management and relief. At WHY.EDU.VN, we’re dedicated to offering comprehensive, reliable information to guide you through your health concerns. Remember, addressing your symptoms with a healthcare professional is a crucial step toward improving your well-being.
Do you have more questions about anal pain or other health concerns? Don’t hesitate to visit WHY.EDU.VN to ask our experts and find the answers you need. Our team is committed to providing accurate and accessible information to help you make informed decisions about your health.
Address: 101 Curiosity Lane, Answer Town, CA 90210, United States
WhatsApp: +1 (213) 555-0101
Website: why.edu.vn
