Why Do We Have Itches? Itching, or pruritus, is a common and often frustrating sensation. WHY.EDU.VN delves into the science behind why our skin itches, exploring the critical protective function it serves and the complex neural pathways involved, offering relief through understanding skin irritations and potential therapeutic interventions. Discover more insights on managing skin discomfort and itch relief with our comprehensive guides, featuring the latest research and expert advice.
1. The Protective Role of Itching
Itching, or pruritus, serves a crucial protective function, alerting us to potential threats or irritants on our skin. This sensation prompts us to scratch, which can dislodge insects, remove irritants, or otherwise mitigate potential harm. It’s our body’s way of saying, “Hey, something’s not right here!”
1.1. The Body’s Defense Mechanism
Itching acts as a defense mechanism, prompting us to remove harmful substances or parasites from our skin. Think of it as an early warning system.
- Removing Irritants: Scratching helps dislodge substances like pollen, dust, or insect debris that can cause irritation.
- Detecting Parasites: The sensation of an itch can alert us to the presence of tiny parasites like mites or fleas, prompting us to remove them before they cause further harm.
- Preventing Infections: By addressing the source of the itch, we can prevent minor skin irritations from escalating into more serious infections.
1.2. Scratching and Its Consequences
While scratching can provide temporary relief, it can also lead to skin damage and potential infections. Understanding this balance is key to managing itches effectively.
| Consequence | Description |
|---|---|
| Skin Damage | Vigorous scratching can break the skin, leading to abrasions, cuts, and open wounds, which are susceptible to bacterial or fungal infections. This damage can disrupt the skin’s natural barrier, making it more vulnerable to future irritants and allergens, perpetuating the itch-scratch cycle. |
| Infection Risk | Broken skin provides an entry point for bacteria and other pathogens. Infections can manifest as redness, swelling, pus, and increased pain or discomfort. In severe cases, untreated infections can spread beyond the skin and cause systemic illness. It’s crucial to keep scratched areas clean and protected to minimize the risk of infection. |
| Chronic Itch Cycle | The relief from scratching is often short-lived, as it can trigger the release of inflammatory substances in the skin, leading to more itching. This creates a vicious cycle where the more you scratch, the more you itch. Over time, this cycle can lead to thickened, leathery skin (lichenification) and persistent itching that is difficult to resolve. Breaking this cycle often requires addressing the underlying cause of the itch and implementing strategies to manage the urge to scratch. |
 Person scratching arm to relieve itch
Person scratching arm to relieve itch
2. Neural Pathways of Itch Sensation
The neural pathways responsible for itch sensation are complex, involving specialized nerve cells and signaling molecules that transmit signals from the skin to the brain. This intricate process allows us to perceive and respond to itchy stimuli.
2.1. Specialized Nerve Cells
Specific nerve cells in the skin, called pruriceptors, are responsible for detecting and transmitting itch signals. These cells are highly sensitive to various stimuli, including mechanical, chemical, and thermal triggers.
- Mechanical Stimuli: Light touch or pressure on the skin can activate pruriceptors, leading to the sensation of itch.
- Chemical Stimuli: Substances like histamine, released during allergic reactions, can bind to receptors on pruriceptors, triggering itch signals.
- Thermal Stimuli: Changes in temperature, such as heat or cold, can also activate pruriceptors and contribute to the sensation of itch.
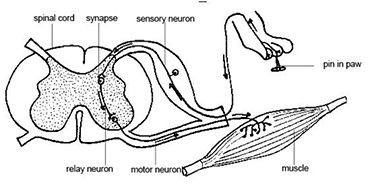
2.2. Role of the Spinal Cord
The spinal cord acts as a relay station, transmitting itch signals from the skin to the brain. Within the spinal cord, specialized interneurons process and modulate these signals before they reach higher brain centers.
2.3. Brain’s Perception of Itch
Different brain regions, including the somatosensory cortex and anterior cingulate cortex, are involved in processing and interpreting itch signals. These regions help us identify the location, intensity, and emotional aspects of the itch sensation.
3. Distinguishing Between Itch and Touch
One of the intriguing aspects of itch sensation is how the body distinguishes between harmless touch and itch-inducing stimuli. This involves specialized neural pathways and inhibitory mechanisms that prevent us from constantly scratching.
3.1. The Role of Inhibitory Neurons
Inhibitory neurons in the spinal cord play a critical role in suppressing itch signals. These neurons act as gatekeepers, preventing excessive or unnecessary itch sensations from reaching the brain.
3.2. The “Gate Control” Theory
The gate control theory proposes that non-painful input, such as gentle touch, can close the “gate” to painful or itchy sensations. This explains why rubbing or applying pressure to an itchy area can sometimes provide relief.
3.3. How the Brain Differentiates
The brain uses a combination of factors, including the type of nerve fibers activated, the intensity of the signal, and the context of the stimulus, to differentiate between itch and touch. This allows us to respond appropriately to different types of sensory input.
4. Chronic Itch and Its Causes
Chronic itch, defined as persistent itching lasting for more than six weeks, can significantly impact quality of life. It is often associated with underlying medical conditions, skin disorders, or neurological issues.
4.1. Skin Conditions
Several skin conditions, such as eczema, psoriasis, and dermatitis, are common causes of chronic itch. These conditions disrupt the skin’s barrier function, leading to inflammation and persistent itching.
| Skin Condition | Description |
|---|---|
| Eczema | A chronic inflammatory skin condition characterized by dry, itchy, and inflamed skin. Eczema can affect people of all ages and is often associated with allergies or asthma. The itching can be intense and persistent, leading to scratching that further damages the skin and perpetuates the itch-scratch cycle. |
| Psoriasis | A chronic autoimmune disease that causes skin cells to grow too quickly, resulting in thick, red, and scaly patches. Psoriasis can occur anywhere on the body and is often associated with itching, burning, and stinging sensations. The itching can be severe and debilitating, significantly impacting quality of life. |
| Dermatitis | A general term for skin inflammation, which can be caused by various factors, including allergies, irritants, and infections. Dermatitis can manifest as redness, itching, swelling, and blisters. The itching associated with dermatitis can be localized or widespread and may be accompanied by other symptoms, such as pain or tenderness. Identifying and avoiding triggers is crucial for managing dermatitis and alleviating itching. |
4.2. Systemic Diseases
Underlying medical conditions, such as kidney disease, liver disease, and thyroid disorders, can also cause chronic itch. These conditions can disrupt normal bodily functions and lead to the release of itch-inducing substances.
4.3. Neurological Disorders
Neurological conditions, such as multiple sclerosis and nerve damage, can affect the neural pathways involved in itch sensation, leading to chronic itch. In these cases, the itch may not be related to any specific skin condition.
5. Chemical, Contagious, and Psychological Itch
Itching can be triggered by various factors, including chemical irritants, psychological cues, and even the sight of others scratching. Understanding these different types of itch can help us manage and alleviate them effectively.
5.1. Chemical Itch
Chemical itch is caused by substances that irritate the skin or trigger an allergic reaction. Common culprits include insect bites, certain medications, and harsh chemicals found in soaps or detergents.
5.2. Contagious Itch
Contagious itch refers to the phenomenon where seeing or hearing about others scratching can trigger the urge to scratch oneself. This is thought to be due to mirror neurons in the brain, which activate when we observe the actions of others.
5.3. Psychological Itch
Psychological factors, such as stress, anxiety, and depression, can also contribute to itching. In some cases, the itch may not have any underlying physical cause but is instead a manifestation of emotional distress.
6. The Relationship Between Itch and Pain
Itch and pain share some overlapping neural pathways, and there is a complex relationship between the two sensations. In some cases, pain can suppress itch, while in others, it can exacerbate it.
6.1. Overlapping Neural Pathways
Both itch and pain signals are transmitted through the spinal cord to the brain via similar neural pathways. This overlap may explain why scratching, which induces mild pain, can temporarily relieve itching.
6.2. Pain as a Counter-Irritant
The sensation of pain can sometimes override the sensation of itch. This is why applying a cold compress or using a topical analgesic can provide relief from itching.
6.3. The Itch-Scratch Cycle
While scratching can provide temporary relief, it can also lead to skin damage and inflammation, which in turn can exacerbate itching. This creates a vicious cycle that can be difficult to break.
7. Current Research on Itch
Ongoing research continues to shed light on the complex mechanisms underlying itch sensation. Scientists are exploring new targets for therapeutic interventions and developing innovative treatments for chronic itch.
7.1. Identifying Key Molecules
Researchers are working to identify specific molecules and receptors involved in itch transmission. This knowledge could lead to the development of targeted therapies that block itch signals without affecting other sensory functions.
7.2. Genetic Studies
Genetic studies are helping to identify genes that may predispose individuals to chronic itch. This could lead to personalized treatments based on an individual’s genetic profile.
7.3. Novel Therapies
Novel therapies, such as monoclonal antibodies and gene therapy, are being investigated as potential treatments for chronic itch. These approaches aim to target specific molecules or pathways involved in itch sensation.
8. Understanding Pruritus: More Than Just an Itch
Pruritus, the medical term for itch, is a symptom that can arise from various underlying conditions. It’s more than just an annoyance; it’s a signal from your body that something needs attention. Let’s delve into the causes, diagnosis, and management of pruritus to gain a comprehensive understanding.
8.1. Diverse Causes of Pruritus
Pruritus can stem from a wide array of causes, ranging from skin conditions to systemic diseases. Identifying the root cause is crucial for effective management.
| Cause Category | Examples |
|---|---|
| Dermatological | Eczema, psoriasis, contact dermatitis, urticaria (hives), fungal infections, parasitic infestations (e.g., scabies) |
| Systemic Diseases | Chronic kidney disease, liver disease (e.g., cholestasis), thyroid disorders (hypo- or hyperthyroidism), iron deficiency anemia, polycythemia vera, certain cancers (e.g., leukemia, lymphoma) |
| Neurological | Multiple sclerosis, diabetic neuropathy, postherpetic neuralgia, nerve compression or damage |
| Psychiatric | Anxiety, depression, obsessive-compulsive disorder, stress |
| Medications | Opioids, antibiotics, antifungals, statins, ACE inhibitors, diuretics |
| Pregnancy | Pruritus gravidarum (itching during pregnancy), cholestasis of pregnancy |
| Idiopathic | Pruritus of unknown origin, where no underlying cause can be identified despite thorough investigation. |
| Environmental Factors | Dry skin (xerosis), insect bites, allergic reactions to plants (e.g., poison ivy), exposure to irritants (e.g., detergents, chemicals) |
8.2. Diagnostic Approaches
Diagnosing the cause of pruritus involves a comprehensive evaluation that may include medical history, physical examination, and various diagnostic tests.
- Medical History:
- Detailed information about the onset, duration, location, and severity of itching.
- History of skin conditions, allergies, and systemic diseases.
- Current medications and supplements.
- Family history of skin or allergic disorders.
- Lifestyle factors, such as occupation, hobbies, and environmental exposures.
- Physical Examination:
- Thorough examination of the skin to identify any visible lesions, rashes, or signs of irritation.
- Assessment of skin dryness, texture, and color.
- Evaluation of lymph nodes for enlargement.
- Diagnostic Tests:
- Blood Tests: Complete blood count (CBC), liver function tests (LFTs), kidney function tests (KFTs), thyroid function tests (TFTs), iron studies, and tests for specific antibodies or markers of systemic diseases.
- Skin Biopsy: Examination of a small skin sample under a microscope to identify specific skin conditions or infections.
- Allergy Testing: Skin prick tests or blood tests to identify specific allergens that may be triggering the itching.
- Patch Testing: Application of various substances to the skin to identify potential contact allergens.
- Imaging Studies: X-rays, CT scans, or MRIs to evaluate for underlying systemic diseases or neurological conditions.
8.3. Management Strategies
Managing pruritus involves a multifaceted approach that addresses the underlying cause, alleviates symptoms, and prevents complications.
- Treating the Underlying Cause:
- Addressing the root cause of pruritus is essential for long-term relief. This may involve treating skin conditions with topical or systemic medications, managing systemic diseases with appropriate therapies, or adjusting medications that are causing itching.
- Symptomatic Relief:
- Topical Treatments: Emollients (moisturizers) to hydrate dry skin, topical corticosteroids to reduce inflammation, and topical antihistamines or calamine lotion to relieve itching.
- Oral Medications: Antihistamines to block histamine release and reduce itching, corticosteroids to reduce inflammation, and antidepressants or anti-anxiety medications to manage psychological factors contributing to pruritus.
- Cooling Measures: Applying cold compresses or taking cool baths to soothe the skin and reduce itching.
- Lifestyle Modifications:
- Avoid Irritants: Identifying and avoiding substances that irritate the skin, such as harsh soaps, detergents, and chemicals.
- Gentle Skin Care: Using mild, fragrance-free skin care products and patting the skin dry after bathing.
- Loose Clothing: Wearing loose-fitting, breathable clothing to minimize friction and irritation.
- Stress Management: Practicing relaxation techniques, such as meditation, yoga, or deep breathing exercises, to reduce stress and anxiety.
- Advanced Therapies:
- Phototherapy: Exposure to ultraviolet (UV) light to reduce inflammation and itching.
- Nerve Blocks: Injection of local anesthetics to block nerve signals and relieve localized itching.
- Emerging Treatments: Investigational therapies, such as monoclonal antibodies and JAK inhibitors, that target specific molecules involved in itch pathways.
9. Debunking Common Myths About Itching
Itching is often surrounded by myths and misconceptions that can lead to ineffective or even harmful practices. Let’s debunk some common myths to promote accurate understanding and appropriate management.
| Myth | Reality |
|---|---|
| Scratching always makes itching worse | While excessive scratching can indeed exacerbate itching and lead to skin damage, gentle scratching or rubbing can sometimes provide temporary relief by activating nerve fibers that inhibit itch signals. However, it’s essential to avoid vigorous scratching that breaks the skin and perpetuates the itch-scratch cycle. |
| Itching is always caused by allergies | Allergies are a common cause of itching, but pruritus can arise from numerous other factors, including skin conditions, systemic diseases, neurological disorders, medications, and psychological factors. It’s crucial to consider the full range of potential causes when evaluating and managing itching. |
| Over-the-counter creams always work | Over-the-counter creams can provide relief for mild itching caused by dry skin, insect bites, or mild allergic reactions. However, they may not be effective for more severe or persistent itching, especially when it stems from an underlying medical condition. In such cases, prescription medications or other medical interventions may be necessary. |
| Itching is purely physical | While many cases of itching have a physical basis, psychological factors, such as stress, anxiety, and depression, can significantly contribute to the sensation of itch. In some cases, itching may be primarily psychogenic, meaning that it originates from psychological distress rather than a physical cause. Addressing these psychological factors through therapy, relaxation techniques, or medications can be an essential part of managing chronic itching. |
| All itches are the same | Itching can vary significantly in its quality, intensity, and distribution. Some itches are localized to a specific area, while others are more generalized. Some itches are described as burning, stinging, or crawling sensations. The characteristics of the itch can provide clues about the underlying cause and guide appropriate management strategies. |
10. Innovations in Itch Research and Treatment
The field of itch research is rapidly evolving, with ongoing efforts to develop innovative treatments that target specific itch pathways and provide more effective relief.
10.1. Targeted Therapies
Researchers are identifying specific molecules and receptors involved in itch transmission, paving the way for targeted therapies that selectively block itch signals without affecting other sensory functions.
10.2. Biologic Medications
Biologic medications, such as monoclonal antibodies, are being developed to target specific immune system components that contribute to inflammation and itching in conditions like eczema and psoriasis.
10.3. Neuromodulation Techniques
Neuromodulation techniques, such as spinal cord stimulation and transcranial magnetic stimulation, are being explored as potential treatments for chronic neuropathic itch.
10.4. Gene Therapy
Gene therapy approaches are being investigated to correct genetic defects that may predispose individuals to chronic itch.
Understanding why we have itches involves delving into the intricate interplay of neural pathways, skin conditions, and various triggers. From the protective role of itching to the complexities of chronic pruritus, ongoing research continues to unveil new insights and potential treatments.
If you’re struggling to find reliable answers to your health questions, or if you’re overwhelmed by the sheer volume of information available online, WHY.EDU.VN is here to help. We connect you with experts who can provide clear, accurate, and trustworthy information tailored to your specific needs.
Don’t let uncertainty keep you scratching your head. Visit why.edu.vn at 101 Curiosity Lane, Answer Town, CA 90210, United States or contact us via WhatsApp at +1 (213) 555-0101 to ask your questions and discover a world of knowledge. Let us guide you to the answers you’ve been searching for.
Frequently Asked Questions (FAQ)
1. Why does scratching make an itch feel better temporarily?
Scratching provides temporary relief by activating pain receptors in the skin, which can override the itch sensation. However, this relief is short-lived and can lead to further skin damage.
2. Can stress cause itching?
Yes, stress, anxiety, and other psychological factors can contribute to itching. In some cases, the itch may not have an underlying physical cause but is instead a manifestation of emotional distress.
3. What are some common causes of chronic itch?
Common causes of chronic itch include skin conditions like eczema and psoriasis, systemic diseases like kidney and liver disease, and neurological disorders.
4. How can I relieve itching without scratching?
Applying a cold compress, using topical creams with menthol or calamine, and taking antihistamines can help relieve itching without damaging the skin.
5. Is itching contagious?
While the sensation of itching can be triggered by seeing others scratch, itching itself is not contagious. The phenomenon is thought to be due to mirror neurons in the brain.
6. When should I see a doctor for itching?
You should see a doctor for itching if it is severe, persistent, or accompanied by other symptoms such as rash, fever, or weight loss.
7. Can certain foods cause itching?
In some cases, food allergies or sensitivities can trigger itching. Common allergenic foods include nuts, shellfish, and dairy products.
8. What is the role of histamine in itching?
Histamine is a chemical released by the body during allergic reactions. It binds to receptors on nerve cells, triggering the sensation of itch.
9. Are there any natural remedies for itching?
Natural remedies for itching include applying aloe vera gel, oatmeal baths, and using herbal creams with ingredients like chamomile or calendula.
10. How does dry skin contribute to itching?
Dry skin lacks moisture, which can lead to irritation and itching. Keeping the skin well-hydrated with moisturizers can help prevent and relieve itching.
