Talking about poop might not be the most glamorous conversation starter, but it’s a vital aspect of your health. Your stool, or poop, provides valuable insights into your digestive system’s well-being. As experts from why.edu.vn, we’re here to guide you through understanding what your poop color means, particularly if you’ve noticed a blackish green hue. This article will delve into the various shades of stool, focusing on blackish green, to help you understand what’s normal, what’s not, and when to seek medical advice.
Understanding Stool Color: A Rainbow of Meanings
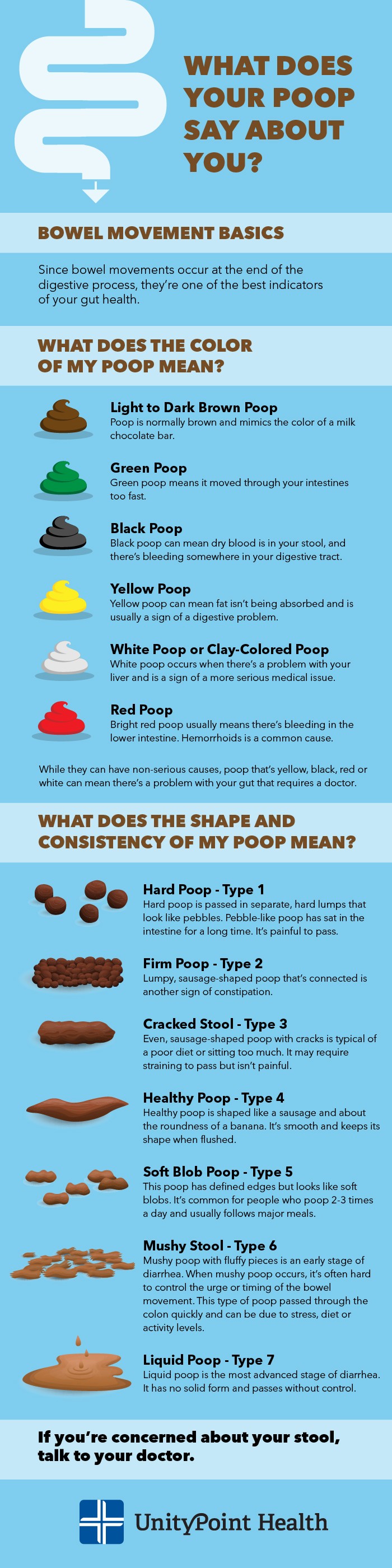
Bowel movements are the final stage of digestion and act as a key indicator of how efficiently your body is processing food. The color of your poop is influenced by several factors, including the speed at which it moves through your intestines, your diet, medications, supplements, and the overall health of your gut.
What is Normal Poop Color?
The benchmark for healthy stool color is brown, ideally resembling the shade of a milk chocolate bar. This characteristic brown color arises from a complex process involving bilirubin, a pigment produced during the breakdown of hemoglobin in the liver. Bilirubin enters the intestines and, in a healthy digestive system, travels at a normal pace, allowing it to transform stool into its typical brown color.
Decoding Green Poop
Seeing green poop can be surprising, but it’s actually quite common and often has benign causes. Bile, a naturally green fluid produced in the liver and stored in the gallbladder, plays a key role. Bile is present in the intestines alongside stool. If your poop moves through the intestines too quickly, bilirubin and iron don’t have sufficient time to interact and complete the process of turning the stool brown. This rapid transit can leave your poop with a green tint.
Other common reasons for green poop include:
- Diet rich in leafy greens: Consuming large quantities of spinach, kale, or other dark leafy greens can lead to green stool due to the chlorophyll content.
- Iron supplements: Iron supplements can sometimes cause a greenish hue to your poop.
- Antibiotics and medications: Certain antibiotics and other medications can alter gut bacteria or speed up digestion, resulting in green stool.
- Green food dyes: Artificial green food coloring in drinks or processed foods can directly color your poop green.
- Bacterial or viral infections: Infections affecting the gastrointestinal tract can sometimes cause changes in stool color, including green.
- Gastrointestinal disorders: Conditions like Crohn’s disease or celiac disease can affect digestion and potentially lead to green stool.
The Concern of Black Poop
Black stool is a more serious sign and often warrants medical attention. It can indicate the presence of dried blood in your poop, suggesting bleeding in the upper gastrointestinal tract. When bleeding occurs higher up in the digestive system, the blood has time to be digested and oxidized, turning it black as it travels through the intestines. If you notice black stool, it’s crucial to consult your doctor promptly as it could be a sign of a significant digestive issue, such as ulcers, gastritis, or tumors in the upper GI tract.
However, not all black poop is due to bleeding. Other, less concerning reasons for black stool include:
- Iron supplements: Similar to causing green stool, iron supplements can also lead to black poop, especially if taken in higher doses.
- Black foods: Eating large amounts of black licorice, blueberries, or dark-colored foods can temporarily darken your stool.
- Bismuth subsalicylate (Pepto-Bismol): This over-the-counter medication, commonly used for upset stomach and diarrhea, contains bismuth subsalicylate, which can cause black stool as a side effect.
Blackish Green Poop: A Combination?
Now, let’s address the specific question: “Why Is My Poop Blackish Green?” Blackish green stool is likely a combination of factors that can cause both black and green stool separately.
It could indicate:
- Dark Green Stool Appearing Blackish: Very dark green stool, especially under certain lighting conditions, might appear blackish green. This could be due to dietary factors, rapid bowel transit, or medications that cause green stool, as mentioned earlier.
- Early Stages of Black Stool (Blood) Mixed with Green Stool Causes: In some cases, blackish green stool might be an early indication of upper GI bleeding where the blood hasn’t fully turned tarry black yet, mixed with factors that are simultaneously causing green stool (like rapid transit or green vegetables in the diet). This scenario is less common but more concerning and requires medical evaluation.
- Iron Supplementation: Iron supplements can sometimes result in stool that is not purely black, but a very dark green or blackish green, depending on the dosage and individual digestion.
To determine the cause of blackish green poop, consider the following:
- Diet: Have you recently eaten a lot of dark leafy greens or foods with green or black food coloring?
- Medications and Supplements: Are you taking iron supplements, antibiotics, or bismuth subsalicylate medications?
- Other Symptoms: Are you experiencing any other symptoms like abdominal pain, nausea, vomiting, weakness, or dizziness? These symptoms, especially in conjunction with blackish green stool, could point towards a more serious issue requiring medical attention.
If you are unsure about the cause of your blackish green stool, especially if it persists or is accompanied by other symptoms, it is always best to consult a healthcare professional to rule out any underlying medical conditions.
 What is Your Poop Trying to Tell You article
What is Your Poop Trying to Tell You article
An infographic illustrating various stool colors and textures, emphasizing that changes in poop can indicate digestive health status.
Other Stool Colors: Yellow, Pale White, and Red
While blackish green is a key focus, understanding other abnormal stool colors provides a broader picture of digestive health:
- Yellow Poop: Yellow stool often occurs when fat is not properly absorbed. This malabsorption can be due to infections (like parasites), illnesses, or congenital conditions affecting the pancreas. Persistent yellow poop, especially lasting more than two days, warrants a doctor’s visit.
- Pale White Poop: Pale, white, or clay-colored stool suggests a lack of bile salts in the stool. This can be caused by bile duct blockages, gallstones, or liver problems. Pale stool is a serious sign and requires medical attention, especially if it lasts for more than two days.
- Red Poop: Bright red stool usually indicates bleeding in the lower digestive tract, often from hemorrhoids. However, it can also signal more serious conditions like inflammatory bowel disease, diverticulitis, or infections. While red food dyes can temporarily color stool red, any persistent red color or blood in stool requires medical evaluation.
What Does the Shape and Consistency of My Stool Say?
Beyond color, the shape and consistency of your poop offer further clues about your digestive health. These factors are influenced by diet, hydration, medications, activity levels, and the time stool spends in the intestines.
Hard Poop – Type 1
Hard, pebble-like poop is a classic sign of constipation. This type of stool has spent an extended period in the large intestine, leading to excessive water removal, resulting in hard, separate lumps.
Firm Poop – Type 2
Lumpy, sausage-shaped but firm poop also indicates constipation. It’s been in the intestines too long but hasn’t become as dehydrated as type 1. This type can be painful to pass due to its size and firmness.
Cracked Poop – Type 3
Sausage-shaped poop with cracks on the surface is often linked to a less-than-ideal diet or sedentary lifestyle. It suggests mild constipation and has spent about a week in the bowels.
Healthy Poop – Type 4
The gold standard! Healthy poop is sausage-shaped, smooth and soft, about the width of a banana, and 4-8 inches long. It’s easy to pass and indicates a balanced digestive system.
Soft Blob Poop – Type 5
Soft blobs with defined edges suggest slightly loose stool, often seen in people with more frequent bowel movements (2-3 times daily), commonly after meals.
Mushy Poop – Type 6
Mushy, fluffy, pudding-like stool is an early stage of diarrhea. It indicates rapid transit through the colon, often due to stress, dietary changes, or increased activity.
Liquid Poop – Type 7
Liquid diarrhea is the most advanced stage of diarrhea, with no solid form and often passed urgently. It results from irritation in the small intestine, causing fluids to be flushed out rapidly.
When to Be Concerned and Seek Medical Advice
It’s normal to experience occasional variations in stool color and consistency. However, certain changes should prompt you to seek medical advice.
Consult your doctor if you experience:
- Black stool, especially if it’s tarry and sticky.
- Blackish green stool that persists or is accompanied by other symptoms.
- Red stool or blood in your stool.
- Pale white or clay-colored stool.
- Yellow stool lasting more than two days.
- Persistent diarrhea (Type 6 or 7) lasting more than a couple of days.
- Severe constipation (Type 1 or 2) lasting more than a week.
- Significant changes in bowel habits that last for more than two weeks.
- Abdominal pain, cramping, nausea, vomiting, or unexplained weight loss along with changes in stool.
Your doctor can evaluate your symptoms, medical history, and perform any necessary tests to determine the cause of your stool changes and recommend appropriate treatment. Don’t hesitate to discuss your concerns about your poop – it’s a crucial indicator of your digestive health, and early detection of any issues can lead to better outcomes.