Coughing is a common reflex, and it’s often the first sign that something is amiss with our health. A fleeting cough might be dismissed as simply “something going down the wrong pipe.” A cough that lingers for a few days might suggest a common cold or the flu. But what about when you find yourself coughing persistently for weeks, yet you don’t feel sick in other ways? This can be perplexing and even concerning. You might wonder, “Why Am I Coughing So Much But Not Sick?”
For many, a chronic cough can trigger anxieties, even leading to worries about serious conditions. But is a persistent cough necessarily a sign of severe illness? And if not, what are the common culprits behind a cough that just won’t quit when you otherwise feel healthy? Let’s delve into the world of coughs to understand why you might be experiencing this frustrating symptom and what you can do about it.
What Exactly Is a Cough?
While often viewed as an annoying symptom, coughing is actually a vital defense mechanism of our body. Think of it as your respiratory system’s way of clearing out unwanted irritants. Coughing is designed to expel mucus, germs, and foreign particles from your airways, ultimately protecting your lungs from infection and inflammation.
The process of coughing is quite intricate. It begins with a deep inhalation, drawing air into your lungs. Then, the glottis, which acts like a valve on your trachea (windpipe), snaps shut. Following this, the muscles in your chest, abdomen, and diaphragm forcefully contract. Normally, these muscles facilitate gentle breathing, pushing air out through the nose and mouth. However, with the glottis closed, the air is trapped, leading to a build-up of significant pressure in your respiratory passages. Finally, the glottis opens abruptly, and air rushes out with tremendous force. This rapid expulsion of air, traveling at near-sonic speeds, is what creates the characteristic sound we recognize as a cough.
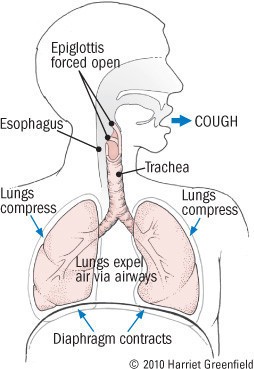 Illustration depicting the anatomy of a cough, showing lungs and the mechanics of air expulsion.
Illustration depicting the anatomy of a cough, showing lungs and the mechanics of air expulsion.
Coughs can be voluntary, something we consciously initiate, or involuntary reflexes triggered by nerve stimulation in the larynx (voice box) and respiratory tract. These nerves can be irritated by a wide range of factors, including infections, allergies, cold air, tumors, chemical irritants like smoke, physical irritants such as dust, or even normal bodily fluids like nasal mucus or stomach acid. Given this sensitivity, it’s easy to see why so many things can provoke a cough.
The Puzzle of Chronic Cough
Everyone experiences a cough from time to time, and an occasional cough is rarely a cause for concern. Many short-term illnesses, from the common cold and hay fever to bronchitis and pneumonia, are accompanied by coughs. However, these coughs typically resolve within a few days to a couple of weeks as the illness runs its course. In contrast, a chronic cough is defined as a cough that persists for more than three to eight weeks, sometimes dragging on for months or even years.
Chronic cough is a surprisingly common ailment, ranking among the most frequent reasons people seek medical attention. Beyond the worry about the underlying cause, individuals with chronic cough often experience frustration and anxiety, particularly when diagnosis and treatment become prolonged, as is often the case. Coughing can disrupt sleep, leading to fatigue and impaired concentration and work performance. In today’s world, persistent coughing can also impact social interactions. Furthermore, chronic coughing can have physical consequences, ranging from urinary incontinence to fainting and even broken ribs in severe cases. The cumulative impact of medical visits, lost productivity, ineffective remedies, and treatments can also make chronic cough a costly condition.
Unpacking the Reasons Behind a Persistent Cough When You’re “Not Sick”
Smoking is a well-known and significant cause of chronic cough. Most smokers will eventually develop a chronic “smoker’s cough” due to chemical irritation from tobacco smoke. However, these same harmful chemicals can also lead to more serious conditions like chronic bronchitis, emphysema, pneumonia, and lung cancer, making a chronic cough in smokers a significant health concern.
But what about non-smokers who find themselves asking, “Why am I coughing so much but not sick?” Fortunately, in non-smokers, the majority of chronic coughs are attributed to benign conditions. While “benign” is reassuring, a persistent cough can still be bothersome, causing worry, embarrassment, and exhaustion. This is why it’s essential to diagnose and manage chronic coughs before they become a long-term issue.
Numerous conditions can trigger a recurring, lingering cough, but a significant portion are due to just a few common culprits. These include:
- Postnasal drip (Upper Airway Cough Syndrome – UACS): This is often the most common reason for a chronic cough in individuals who otherwise feel well.
- Asthma: Especially cough-variant asthma, where coughing is the primary symptom, not wheezing.
- Gastroesophageal Reflux Disease (GERD): Stomach acid refluxing into the esophagus can trigger a cough reflex, sometimes without typical heartburn symptoms.
- ACE Inhibitors: These medications, used for high blood pressure and heart failure, are known to cause cough in some individuals.
- Chronic Bronchitis: While more common in smokers, it can also occur in non-smokers due to environmental irritants.
It’s important to note that many individuals might have more than one of these contributing factors. However, in non-smokers, postnasal drip, asthma, and GERD, either alone or in combination, are responsible for the vast majority of chronic coughs when they are “not sick” with an acute illness.
| Persistent Cough: Major Causes |
|---|
| Common Causes of a Nagging Cough |
| * Postnasal drip (Upper Airway Cough Syndrome) |
| * Asthma (including cough-variant asthma) |
| * Gastroesophageal Reflux Disease (GERD) |
| * ACE Inhibitors (medication side effect) |
| Less Common Causes of a Nagging Cough |
| * Airborne environmental irritants |
| * Aspiration during swallowing |
| * Heart failure |
| * Lung infections |
| * Pertussis (whooping cough) |
| * Lung cancer |
| * Other lung diseases |
| * Psychological disorders |
| Common in Smokers |
| * Tobacco smoke itself |
| * Lung cancer |
| * Lung infections |
Let’s explore some of these major causes in more detail, especially those relevant to the question, “Why am I coughing so much but not sick?”.
1. Postnasal Drip (Upper Airway Cough Syndrome – UACS):
Your nose plays a critical role in conditioning the air you breathe before it reaches your lungs. It warms cool air, humidifies dry air, and filters out particles from dirty air. Nasal membranes achieve this by producing mucus that is warm, moist, and sticky.
However, these membranes can be irritated by viruses, allergies, sinusitis, dust, and airborne chemicals. When irritated, they produce excessive mucus that is thinner and more watery than normal. While some of this mucus drains out of the nose, causing a runny nose, some drips down the back of the throat. This postnasal drip can irritate the nerves in the nasopharynx, triggering a cough reflex. Sometimes, postnasal drip persists even after a viral upper respiratory infection has resolved, leading to what’s called a post-infectious cough.
People with postnasal drip often cough more at night and may feel a tickling sensation in the back of their throat. However, coughing can occur throughout the day, and the throat may or may not feel sore.
Treating postnasal drip is often the first step in addressing a chronic cough. Over-the-counter decongestant or antihistamine medications are commonly used. These medications work by reducing mucus production or drying up nasal passages. While generally effective and safe, they can have side effects. Decongestants might cause a racing heart or jitteriness, while antihistamines can cause drowsiness. Individuals with benign prostatic hyperplasia (BPH) should be cautious with decongestants, and antihistamines can occasionally trigger glaucoma. Always read medication instructions carefully.
Home remedies can also provide relief. Steam inhalation from a hot shower or kettle is a simple and effective method. Nasal saline irrigations can help clear out irritants and excess mucus. You can use over-the-counter saline sprays or make your own solution by dissolving ⅛ teaspoon of table salt per cup of water. Sniffing this saline solution gently can help cleanse nasal passages. Repeat saline irrigations one to three times daily if they provide relief.
Postnasal drip is a leading cause of persistent cough, especially when you otherwise feel well.
2. Asthma (Cough-Variant Asthma):
Asthma is typically associated with wheezing and shortness of breath. However, not all asthma sufferers experience wheezing. In some cases, coughing is the predominant, or even sole, symptom. This is known as cough-variant asthma.
Asthma is characterized by bronchospasm, a temporary and reversible narrowing of the airways in the lungs. This narrowing often produces a whistling or wheezing sound as air passes through constricted passages. While typical asthma symptoms include excessive mucus production, shortness of breath, and cough, cough-variant asthma presents primarily as a cough.
Cough-variant asthma typically manifests as a persistent, dry cough that can occur at any time but may worsen at night. Triggers like allergens, dust, cold air, and exercise can often exacerbate coughing episodes.
If asthma is suspected as the cause of a chronic cough, doctors may perform pulmonary function tests to confirm the diagnosis. If these tests are inconclusive, a methacholine challenge test might be conducted, where a small dose of methacholine, a bronchoconstrictor, is inhaled to see if it triggers wheezing, a common response in asthmatics.
Another diagnostic approach is to assess the cough’s response to asthma treatment. Doctors might prescribe a bronchodilator inhaler like albuterol (Proventil, Ventolin), which provides short-term relief. Additionally, inhaled corticosteroids such as fluticasone (Flovent), triamcinolone (Azmacort), or budesonide (Pulmicort) might be prescribed for longer-term management.
If you are experiencing a chronic cough and suspect asthma, especially if you notice it worsens with triggers or at night, discuss testing or treatment options with your doctor.
3. Gastroesophageal Reflux Disease (GERD):
Many people are surprised to learn that GERD, commonly known for heartburn, can also cause a cough, even without the presence of heartburn.
GERD occurs when stomach contents, including acid, flow back up into the esophagus instead of moving down into the intestines. While heartburn is the most common symptom, other symptoms like belching, a sour taste in the mouth, and bad breath are also frequent. However, stomach acid can also irritate nerves in the esophagus, triggering the cough reflex, even in the absence of pain or heartburn. In fact, a significant portion of GERD patients, up to one-third, might not experience pain and may only present with a cough, voice changes due to laryngitis, or unexplained sore throats.
Diagnosing GERD as the cause of cough can be challenging when heartburn is absent. Esophageal pH monitoring, involving a probe inserted into the lower esophagus for 24 hours to detect acid reflux, can be used. However, it’s an expensive and somewhat inconvenient procedure.
Similar to other causes of chronic cough, a simpler diagnostic approach is to try GERD treatment. You can start with lifestyle modifications and over-the-counter remedies. Avoid alcohol and foods that commonly trigger GERD, such as chocolate, peppermint, caffeine, garlic, onions, citrus fruits, tomato sauce, and fatty foods. Eat smaller meals and avoid lying down for at least two hours after eating. Taking liquid antacids, particularly at bedtime, and elevating the head of your bed or using a wedge-shaped pillow can help keep stomach contents down during sleep.
If lifestyle changes are insufficient, over-the-counter acid suppressants can be added. Options include cimetidine (Tagamet), famotidine (Pepcid), omeprazole (Prilosec), and lansoprazole (Prevacid). Generic versions are equally effective and often more affordable. Stronger prescription-strength acid blockers are also available.
It can take several weeks of consistent treatment to manage GERD effectively. If your cough doesn’t improve after a few weeks of GERD management, it’s likely that another cause is responsible.
4. Chronic Bronchitis and Bronchiectasis:
Chronic bronchitis involves persistent inflammation of the bronchial tubes, leading to airway narrowing and excessive mucus production. It’s most commonly caused by smoking or long-term exposure to industrial air pollutants. Bronchiectasis is another condition resulting from chronic inflammation that damages the bronchial tube walls. Both conditions can lead to a chronic cough.
The most effective treatment for chronic bronchitis is to quit smoking and avoid air pollutants. Doctors may also prescribe corticosteroid inhalers, often combined with a long-acting bronchodilator, to manage symptoms. Individuals with chronic bronchitis are prone to flare-ups, known as COPD exacerbations. These flare-ups are characterized by increased coughing, thicker, darker mucus production, shortness of breath, and fatigue. Treatment for exacerbations typically includes antibiotics and oral corticosteroids like prednisone.
5. ACE Inhibitors:
ACE inhibitors, such as enalapril (Vasotec), lisinopril (Prinivil, Zestril), and others, are widely used to treat high blood pressure and heart failure. They are favored for their effectiveness and generally mild side effect profile. However, a persistent cough is a known side effect, occurring in up to 10% of people taking ACE inhibitors.
The cough typically starts with a throat tickle, followed by a dry cough that can develop anywhere from three weeks to a year after starting the medication. Once it begins, the cough can be persistent and bothersome.
If the cough is mild, some individuals may choose to continue the medication, or switching to a different ACE inhibitor might reduce coughing. However, the only way to completely eliminate an ACE inhibitor-induced cough is to switch to an alternative type of antihypertensive medication. Fortunately, several alternatives are available, including angiotensin-receptor blockers (ARBs) like losartan (Cozaar) and valsartan (Diovan), which have similar benefits to ACE inhibitors but are less likely to cause cough.
| When to Worry About a Constant Cough |
|---|
| While a chronic cough is often not serious, certain warning symptoms warrant prompt medical attention. These include: |
| * Fever, especially if high or prolonged |
| * Copious sputum production |
| * Coughing up blood |
| * Shortness of breath |
| * Weight loss |
| * Weakness, fatigue, loss of appetite |
| * Chest pain not directly caused by coughing |
| * Night sweats |
| * Wheezing |
| If you experience any of these warning signs along with your cough, it’s crucial to seek medical advice promptly to rule out more serious conditions. |
Less Common Reasons for a Lingering Cough
While the “Big Five” causes account for the vast majority of chronic coughs in non-smokers who are otherwise “not sick,” other less common conditions can also be responsible.
- Lung Infections: While most pneumonia cases are acute and require immediate treatment, some lung infections can be slower to develop and cause a persistent cough. Fever is an important indicator of infection.
- Pertussis (Whooping Cough): This respiratory infection can be serious, especially in children not fully vaccinated with the DPT vaccine.
- Heart Disease: Heart failure can sometimes manifest with cough and breathlessness as primary symptoms, mimicking lung disease. The cough in heart failure is often worse when lying flat and may produce thin, frothy white sputum. Leg swelling, fatigue, and exercise intolerance are other associated symptoms.
- Abnormal Swallowing (Aspiration): If food or liquids are aspirated into the airway instead of the esophagus, it can trigger a chronic cough. This is more common in individuals with stroke or neurological disorders affecting swallowing.
- Environmental Irritants: Exposure to airborne irritants like sulfur dioxide, nitric oxide, dust, and molds can trigger a persistent cough. Even dry or cold air can be irritating.
- Lung Cancer: While less common in non-smokers, lung cancer is a serious consideration for persistent cough, especially in smokers or former smokers.
- Stress (Psychogenic Cough): Mental stress can manifest in physical symptoms, including cough. Psychogenic cough may worsen during stressful periods and disappear during sleep.
Navigating Cough Remedies
If you’ve ever walked down the cough and cold medicine aisle in a drugstore, you know there’s a vast array of cough syrups, sprays, tablets, and lozenges promising relief. Many cough remedies contain expectorants like guaifenesin, intended to loosen mucus and make it easier to cough up. However, scientific evidence supporting the effectiveness of expectorants is limited. Staying hydrated and using a humidifier might be equally beneficial.
Cough suppressants, such as dextromethorphan in over-the-counter medications or codeine in prescription syrups, can help reduce the cough reflex for comfort. However, it’s important to remember that coughing serves a purpose, and suppressing it entirely isn’t always advisable.
Medicated lozenges and cough drops often contain ingredients like menthol, camphor, eucalyptus oil, and honey, sometimes with topical anesthetics. Despite their popularity, there’s no strong evidence that medicated cough drops are more effective than regular hard candies in soothing a cough.
| Cough Medicine
