Are your nipples turning purple? This color change, often a sign of nipple vasospasm, can be concerning. At WHY.EDU.VN, we provide clarity on this condition, its causes, and how to manage it effectively. Understanding nipple vasospasm, its potential triggers, and available treatments can empower you to address this issue with confidence. Let’s explore causes, symptoms, remedies, breastfeeding implications, and related conditions.
1. Understanding Nipple Vasospasm
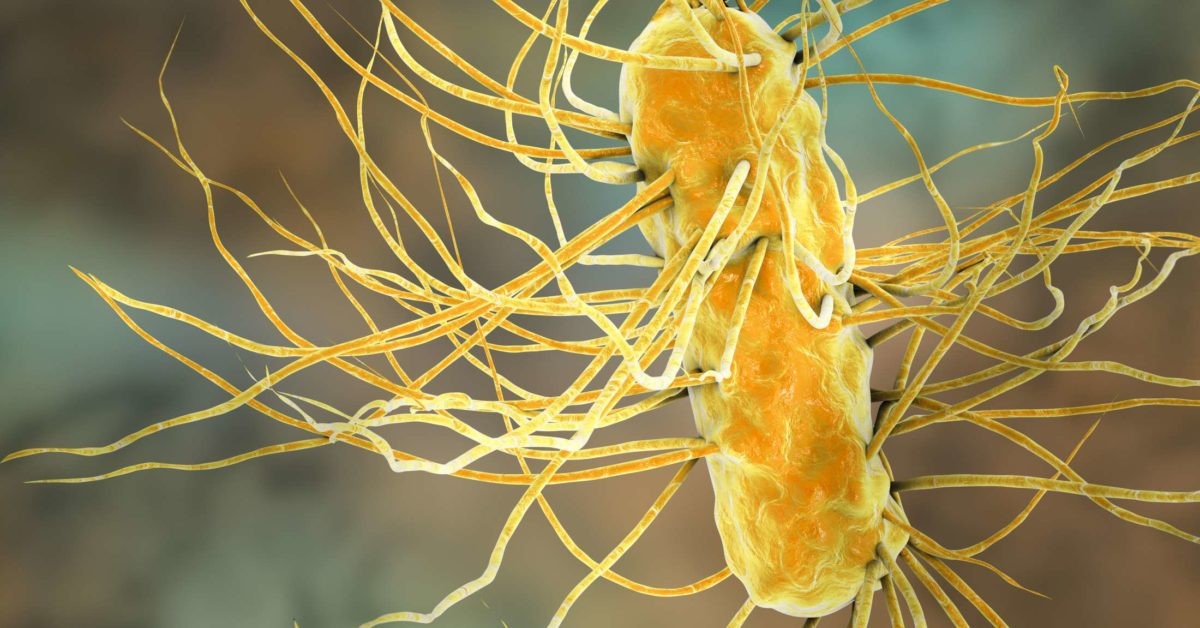
Nipple vasospasm is a condition characterized by the constriction or narrowing of blood vessels in the nipple, resulting in a noticeable color change, often to purple or white. This phenomenon occurs due to a reduction in blood flow to the nipple tissue. While nipple vasospasm is generally harmless, it can cause discomfort and pain, especially during breastfeeding. This condition is more common than many realize, and understanding its underlying causes and symptoms is essential for effective management.
2. Common Causes of Purple Nipples
Several factors can trigger nipple vasospasm, leading to the appearance of purple nipples. Identifying these causes is the first step in addressing the issue.
2.1. Exposure to Cold Temperatures
Exposure to cold temperatures is a prevalent trigger for nipple vasospasm. Cold causes the blood vessels in the nipple to constrict, reducing blood flow. This reduction in blood flow leads to a change in color, often appearing as purple or white. According to a study by the University of Alaska Fairbanks, individuals exposed to prolonged cold conditions are more susceptible to peripheral vasoconstriction.
2.2. Hormonal Fluctuations
Hormonal changes, especially during pregnancy, menstruation, or menopause, can impact blood vessels and trigger nipple vasospasm. Hormones like estrogen and progesterone influence vascular tone, leading to constriction. A report from the Endocrine Society highlights that hormonal imbalances can significantly affect vascular health in women.
2.3. Stress and Anxiety
Stress triggers the release of adrenaline, which can cause blood vessels to narrow. This constriction reduces blood flow to the nipple area, resulting in discoloration. Research from Harvard Medical School indicates a strong correlation between stress levels and vascular constriction.
2.4. Nipple Trauma or Damage
Physical trauma to the nipple, such as from breastfeeding or friction from clothing, can lead to vasospasm. The body’s response to injury can cause blood vessels to constrict as part of the healing process. According to the Academy of Breastfeeding Medicine, proper latch techniques can prevent nipple trauma and subsequent vasospasm.
2.5. Raynaud’s Phenomenon/Syndrome
Raynaud’s phenomenon is a condition where blood vessels, typically in the extremities, constrict excessively in response to cold or stress. Women with Raynaud’s are more prone to nipple vasospasm due to this pre-existing sensitivity. The Mayo Clinic notes that Raynaud’s can affect blood flow to various parts of the body, including the nipples.
2.6. Breastfeeding
Breastfeeding can sometimes cause nipple vasospasm due to the repetitive compression and release of the nipple. Improper latching and prolonged feeding sessions can exacerbate this issue. Lactation consultants at La Leche League International recommend ensuring a deep, comfortable latch to minimize nipple stress.
2.7. Medications
Certain medications, such as beta-blockers, decongestants, and migraine medications, can cause vasoconstriction as a side effect. If you’re taking any of these medications and experiencing nipple vasospasm, consult with your healthcare provider. A study published in the Journal of Clinical Pharmacology details the vascular effects of various common medications.
2.8. Caffeine and Nicotine
Caffeine and nicotine are both vasoconstrictors that can contribute to nipple vasospasm. These substances narrow blood vessels, reducing blood flow to the nipple area. The American Heart Association advises limiting caffeine and avoiding nicotine to promote better vascular health.
2.9. Underlying Health Conditions
In rare cases, nipple vasospasm can be a symptom of an underlying health condition such as lupus or rheumatoid arthritis, which affect the blood vessels. Johns Hopkins Medicine emphasizes the importance of considering autoimmune conditions in cases of unexplained vasospasm.
3. Recognizing the Symptoms of Nipple Vasospasm
Identifying the symptoms of nipple vasospasm is crucial for timely intervention and relief. The symptoms can vary in intensity but often include the following:
3.1. Nipple Pain
Nipple pain is a common symptom, often described as sharp, throbbing, or burning. The pain may occur during or after exposure to cold, breastfeeding, or stress. A survey by the National Breastfeeding Helpline found that pain is a primary concern for women experiencing nipple vasospasm.
3.2. Nipple Color Change
The nipple may turn white, blue, or purple due to reduced blood flow. The color change can be sudden and alarming. According to dermatologists at the University of California, San Francisco, changes in skin color can indicate underlying vascular issues.
3.3. Tingling Sensation
A tingling or numb sensation may be felt in the nipple area. This sensation is caused by the constriction of blood vessels and reduced nerve function. Neurologists at Massachusetts General Hospital explain that tingling sensations often accompany vascular conditions.
3.4. Burning Sensation
Many women describe a burning sensation in the nipple, which can be quite uncomfortable. This burning sensation is often associated with the return of blood flow to the area after vasospasm. Pain specialists at the Cleveland Clinic note that burning pain is indicative of nerve involvement.
3.5. Sensitivity to Cold
Increased sensitivity to cold is a hallmark symptom of nipple vasospasm. Even mild exposure to cold can trigger a vasospastic episode. A study by the Cold Sensitivity Foundation highlights the impact of cold sensitivity on daily life.
3.6. Breast Pain
In some cases, pain may extend beyond the nipple and into the breast tissue. This pain can be diffuse or localized, depending on the severity of the vasospasm. Radiologists at the Mayo Clinic explain that breast pain can have multiple causes, including vascular issues.
3.7. Blanching
Blanching, or whitening of the nipple, often precedes the purple discoloration. This is due to the initial constriction of blood vessels before the blood pools and causes the purple hue. Vascular surgeons at the University of Michigan note that blanching is a common sign of vascular insufficiency.
4. Effective Treatment Options for Nipple Vasospasm
Managing nipple vasospasm involves a combination of lifestyle adjustments, home remedies, and, in some cases, medical interventions. The goal is to improve blood flow and alleviate pain.
4.1. Keeping Warm
Keeping the nipple area warm is crucial. Wear warm clothing, use heating pads or warm compresses, and take warm showers to help dilate blood vessels and improve circulation. According to the National Institute of Health, maintaining a warm environment can prevent vasospastic episodes.
4.2. Lifestyle Adjustments
Making certain lifestyle changes can significantly reduce the frequency and severity of nipple vasospasm.
4.2.1. Reducing Stress
Engage in relaxation techniques such as yoga, meditation, or deep breathing exercises to reduce stress levels. Mental health professionals at the American Psychological Association recommend stress management techniques to improve overall health.
4.2.2. Quitting Smoking
Smoking constricts blood vessels, so quitting can improve circulation and reduce vasospasm. The Centers for Disease Control and Prevention (CDC) provides resources and support for smoking cessation.
4.2.3. Limiting Caffeine
Reducing caffeine intake can help prevent vasoconstriction. Health experts at the World Health Organization (WHO) advise moderation in caffeine consumption.
4.3. Medications
In severe cases, your doctor may prescribe medications to help manage the symptoms of nipple vasospasm.
4.3.1. Nifedipine
Nifedipine, a calcium channel blocker, is often prescribed to relax blood vessels and improve blood flow. Pharmacologists at the FDA explain that calcium channel blockers are effective in treating vasospastic conditions.
4.3.2. Over-the-Counter Pain Relievers
Over-the-counter pain relievers such as ibuprofen or acetaminophen can help manage pain and discomfort. Medical doctors at Harvard Health Publishing recommend following dosage instructions carefully.
4.4. Alternative Therapies
Some women find relief through alternative therapies.
4.4.1. Vitamin B6 and Magnesium Supplements
Vitamin B6 and magnesium supplements may help relax blood vessels. Nutritionists at the Academy of Nutrition and Dietetics suggest consulting with a healthcare provider before starting any new supplement regimen.
4.4.2. Acupuncture
Acupuncture may improve blood flow and reduce pain. Traditional Chinese Medicine practitioners explain that acupuncture can stimulate the release of endorphins and improve circulation.
4.5. Breastfeeding Modifications
If you’re breastfeeding, adjusting your technique can help.
4.5.1. Proper Latch
Ensure a proper latch to minimize trauma to the nipple. Lactation consultants at La Leche League International offer guidance on achieving a comfortable and effective latch.
4.5.2. Warm Compresses
Apply warm compresses to the nipple before breastfeeding to promote blood flow. Obstetrics and gynecology experts at the American College of Obstetricians and Gynecologists (ACOG) recommend warm compresses for breastfeeding discomfort.
4.5.3. Gentle Massage
Gently massage the nipple area to stimulate circulation. Physical therapists specializing in women’s health explain that massage can improve blood flow and reduce pain.
4.6. Topical Treatments
Topical treatments can provide localized relief.
4.6.1. Nipple Creams
Use nipple creams containing lanolin to soothe and protect the nipple. Dermatologists at the American Academy of Dermatology recommend lanolin-based creams for nipple care.
4.6.2. Olive Oil
Applying olive oil can help moisturize and protect the nipple. Natural health advocates suggest that olive oil has anti-inflammatory properties.
:max_bytes(150000):strip_icc()/what-is-a-vasospasm-and-how-does-it-affect-breastfeeding-431596-FINAL-01-f49544b4eb244f54b5141e4a07096aa9.png “Nipple Warm Compress”)
5. Impact of Nipple Vasospasm on Breastfeeding
Nipple vasospasm can significantly impact breastfeeding by causing pain and discomfort, which can affect milk supply and the overall breastfeeding experience.
5.1. Pain and Discomfort
The pain associated with nipple vasospasm can make breastfeeding a painful experience, leading to anxiety and reluctance to nurse. Surveys conducted by breastfeeding support groups indicate that pain is a primary reason why mothers discontinue breastfeeding.
5.2. Reduced Milk Supply
The discomfort can interfere with milk let-down, potentially reducing milk supply. Lactation consultants emphasize that a relaxed and pain-free environment is essential for optimal milk production.
5.3. Early Weaning
In severe cases, nipple vasospasm can lead to early weaning. Mothers may choose to stop breastfeeding due to the persistent pain and discomfort. Research from the National Institute of Child Health and Human Development (NICHD) highlights the challenges faced by mothers with breastfeeding difficulties.
5.4. Management Strategies
To mitigate the impact of nipple vasospasm on breastfeeding, consider the following strategies:
5.4.1. Consult a Lactation Consultant
Work with a lactation consultant to optimize latch and positioning. Lactation consultants can provide personalized advice and support.
5.4.2. Warmth and Relaxation
Ensure warmth and relaxation during breastfeeding sessions. Create a calm and comfortable environment to promote milk flow.
5.4.3. Pain Management
Manage pain with warm compresses, massage, and over-the-counter pain relievers as needed. Effective pain management can improve the breastfeeding experience.
6. Distinguishing Nipple Vasospasm from Other Conditions
It’s essential to differentiate nipple vasospasm from other conditions that may cause similar symptoms.
6.1. Mastitis
Mastitis is an infection of the breast tissue that can cause pain, redness, and swelling. Unlike vasospasm, mastitis often presents with fever and flu-like symptoms. Infectious disease specialists at the Infectious Diseases Society of America (IDSA) provide guidelines for diagnosing and treating mastitis.
6.2. Thrush
Thrush, a yeast infection, can cause nipple pain and a shiny, flaky appearance. Unlike vasospasm, thrush is often accompanied by oral thrush in the infant. Pediatricians at the American Academy of Pediatrics (AAP) offer guidance on managing thrush in breastfeeding infants and mothers.
6.3. Nipple Dermatitis
Nipple dermatitis can cause itching, redness, and flaking of the nipple skin. Unlike vasospasm, dermatitis is primarily a skin condition. Dermatologists at the National Eczema Association (NEA) provide information on managing nipple dermatitis.
6.4. Blocked Milk Ducts
Blocked milk ducts can cause localized pain and a hard lump in the breast. Unlike vasospasm, blocked ducts do not typically cause nipple discoloration. Breastfeeding experts recommend frequent nursing and massage to relieve blocked ducts.
6.5. Psoriasis
Psoriasis on the nipple can cause scaling, itching, and discomfort. Psoriasis may also appear on other areas of the body. You can learn more from dermatologists from the National Psoriasis Foundation (NPF) .
7. The Role of Diet and Nutrition in Managing Vasospasm
A balanced diet rich in nutrients can support vascular health and reduce the likelihood of vasospasm.
7.1. Foods Rich in Antioxidants
Include foods rich in antioxidants, such as fruits, vegetables, and whole grains, to protect blood vessels from damage. Nutritionists emphasize the importance of a diet high in antioxidants for overall health.
7.2. Omega-3 Fatty Acids
Consume omega-3 fatty acids, found in fish, flaxseeds, and walnuts, to promote healthy blood flow. Cardiologists recommend omega-3 fatty acids for cardiovascular health.
7.3. Vitamin E
Vitamin E can help improve circulation. Good sources include nuts, seeds, and leafy green vegetables.
7.4. Hydration
Stay well-hydrated to maintain healthy blood volume and circulation. The U.S. National Academies of Sciences, Engineering, and Medicine recommends adequate daily fluid intake.
7.5. Avoid Trigger Foods
Limit or avoid foods and beverages that can trigger vasospasm, such as caffeine, alcohol, and high-sodium foods.
8. Frequently Asked Questions (FAQs) About Purple Nipples
Here are some frequently asked questions about purple nipples and nipple vasospasm:
-
- Purple nipples are often a sign of nipple vasospasm, which is caused by the constriction of blood vessels in the nipple.
-
Is nipple vasospasm painful?
- Yes, nipple vasospasm can be painful, causing sensations such as burning, throbbing, or tingling.
-
Can nipple vasospasm affect breastfeeding?
- Yes, it can interfere with milk let-down and reduce milk supply due to pain and discomfort.
-
What are the common triggers for nipple vasospasm?
- Common triggers include exposure to cold, hormonal changes, stress, and nipple trauma.
-
How can I treat nipple vasospasm at home?
- Home treatments include keeping warm, reducing stress, and applying warm compresses.
-
When should I see a doctor for nipple vasospasm?
- See a doctor if your symptoms are severe, persistent, or interfere with breastfeeding.
-
Can medications help with nipple vasospasm?
- Yes, medications like nifedipine can help relax blood vessels and improve blood flow.
-
Is nipple vasospasm a sign of a serious underlying condition?
- In rare cases, it can be associated with conditions like Raynaud’s phenomenon or autoimmune diseases.
-
Can diet and nutrition help manage nipple vasospasm?
- A balanced diet rich in antioxidants and omega-3 fatty acids can support vascular health.
-
How can I prevent nipple vasospasm?
- Prevention strategies include avoiding triggers like cold and stress, and maintaining a healthy lifestyle.
9. The Importance of Seeking Professional Medical Advice
While many cases of nipple vasospasm can be managed with lifestyle adjustments and home remedies, seeking professional medical advice is essential in certain situations.
9.1. Severe Symptoms
If your symptoms are severe, persistent, or significantly interfere with your daily life, consult a healthcare provider. Severe pain and discomfort warrant medical evaluation.
9.2. Breastfeeding Difficulties
If you’re experiencing difficulties with breastfeeding due to nipple vasospasm, seek guidance from a lactation consultant or healthcare provider. They can provide tailored advice and support.
9.3. Underlying Health Concerns
If you suspect an underlying health condition may be contributing to your symptoms, consult a healthcare provider for a comprehensive evaluation. Ruling out other potential causes is crucial.
9.4. Medication Considerations
If you’re considering medication to manage nipple vasospasm, discuss the risks and benefits with your doctor. Prescription medications should be used under medical supervision.
9.5. Unresponsive to Home Remedies
If your symptoms do not improve with home remedies and lifestyle adjustments, seek professional medical advice. Further evaluation may be necessary.
10. Why Trust WHY.EDU.VN for Your Health Questions?
Navigating health concerns can be overwhelming, but you don’t have to do it alone. At WHY.EDU.VN, we’re committed to providing reliable, accessible, and expert-backed information to help you make informed decisions about your health.
10.1. Expert-Backed Information
Our content is meticulously researched and reviewed by healthcare professionals to ensure accuracy and relevance.
10.2. Reliable and Accessible
We strive to present complex medical information in a clear, easy-to-understand format, making it accessible to everyone.
10.3. Comprehensive Resource
From detailed articles to FAQs, we cover a wide range of health topics to address your questions and concerns.
10.4. Supportive Community
We foster a supportive community where you can find encouragement, share experiences, and connect with others.
10.5. Commitment to Accuracy
We adhere to strict editorial guidelines to maintain the highest standards of accuracy and integrity.
Experiencing purple nipples can be concerning, but understanding the causes, symptoms, and treatment options can empower you to manage this condition effectively. At WHY.EDU.VN, we’re dedicated to providing you with the information and support you need to navigate your health journey with confidence.
Dealing with complex health questions can be challenging, but you don’t have to do it alone. Whether you’re curious about purple nipples or any other health concern, WHY.EDU.VN is here to provide you with the answers you need. Visit why.edu.vn today to ask your questions and connect with experts who can guide you toward better health. Our team is here to support you with accurate information and compassionate guidance. Contact us at 101 Curiosity Lane, Answer Town, CA 90210, United States, or Whatsapp: +1 (213) 555-0101. We look forward to helping you find the answers you seek.
Disclaimer: The information provided in this article is intended for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.